Key Takeaway:
- PTSD and addiction are strongly linked: People with PTSD are more likely to develop addiction, with substance use often being used as a coping mechanism for PTSD symptoms.
- There are several risk factors that increase the likelihood of both PTSD and addiction, including experiencing traumatic events, social isolation, and having a family history of addiction or mental health issues.
- Integrated treatment approaches are the most effective for treating PTSD and addiction simultaneously, which may include psychotherapy, pharmacotherapy, and other alternative therapies to address the root causes of both disorders.
Are you struggling with PTSD and addiction? Learn how these two conditions are connected and how to seek help to begin the journey to recovery. You don’t have to go through it alone.
Understanding the Link Between PTSD and Addiction
As someone who has personally witnessed the impact of both PTSD and addiction, I know how important it is to understand the connection between the two. In this part of the article, we will be exploring the link between PTSD and addiction in detail.
We will start by defining PTSD and exploring the various ways in which it can manifest itself. From there, we will delve into addiction and its consequences. By the end of this section, you will hopefully have a deeper understanding of the intersection between these two complex issues and how they can affect individuals.

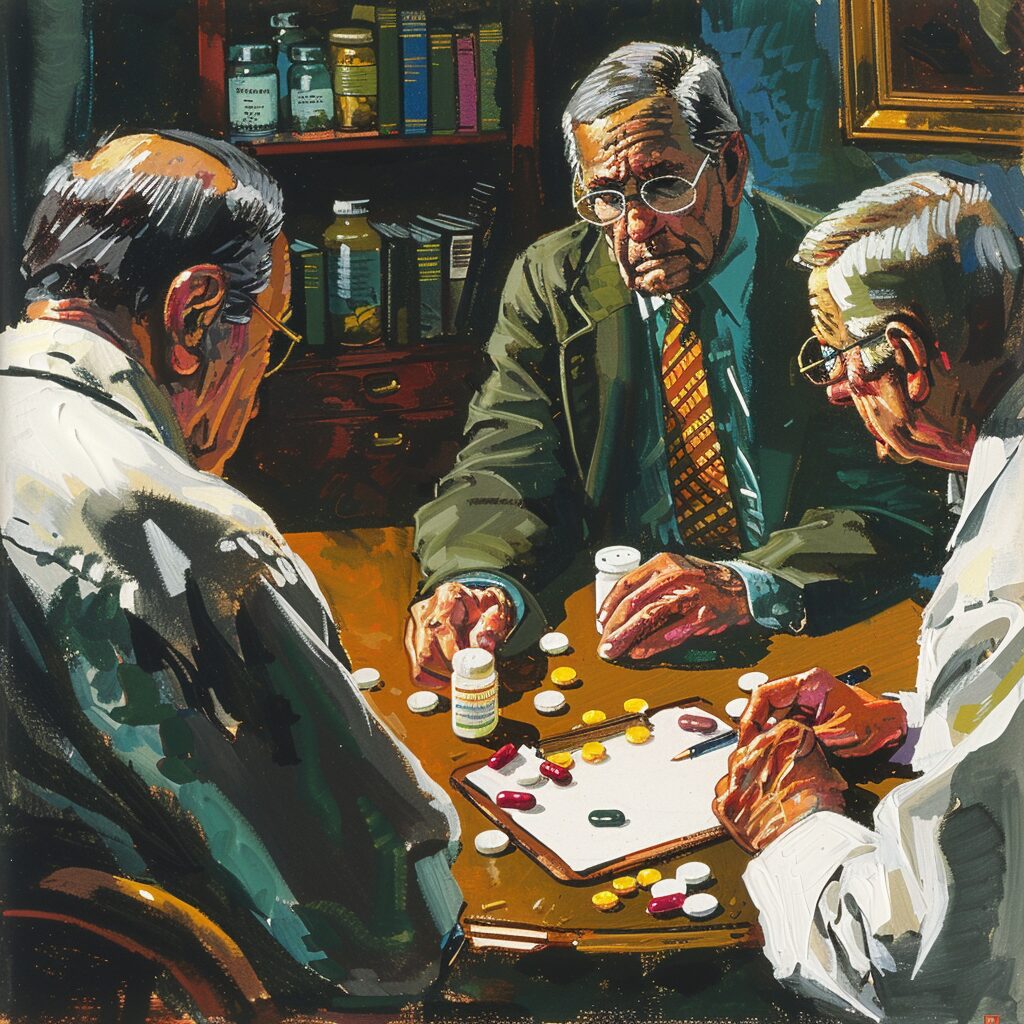
Image credits: www.lantanarecovery.com by James Arnold
Defining PTSD and Its Effects
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after experiencing or witnessing a traumatic event. Its effects are far-reaching and can cause significant distress to those affected by it. This article will explore the implications of PTSD and its connection to addiction.
PTSD works by creating persistent and vivid memories of the traumatic experience, which can lead to flashbacks, nightmares, and intense feelings of anxiety. These symptoms can be triggered by anything that brings back memories of the trauma, leading to avoidance behaviors, social withdrawal, numbness, and emotional detachment. The condition often develops as an adaptive response to extreme stress but can become debilitating if not treated.
People with PTSD have been found to have altered brain structures in areas responsible for memory and emotional regulation. These changes may contribute to their abnormal reactions to trauma-related stimuli or triggers.
Studies have also shown that PTSD increases the risk of developing substance use disorders (SUDs) such as alcoholism or drug addiction. People with PTSD may turn to drugs or alcohol as a way of self-medicating their symptoms or coping with the associated stressors. Unfortunately, this behavior only exacerbates their problem and perpetuates a cycle of addiction.
“I remember getting diagnosed with severe PTSD after a series of events in Iraq where I was deployed during my military service. The effects were devastating – I had trouble holding down jobs, maintaining relationships, and even leaving my apartment became difficult. The flashbacks would come at any time, causing me to relive the events over and over again in my head.”
But it’s important to note that there is hope for people facing these challenges. Effective treatments such as cognitive-behavioral therapy (CBT), medication management, and support groups provide avenues for recovery from both PTSD and SUDs.
The struggle with addiction is a difficult one – especially when combined with a condition like PTSD – but it’s not insurmountable. In the next section, we will delve into addiction and its consequences with an eye towards understanding how these issues intersect.
Identifying Addiction and Its Consequences
The journey from addiction to recovery begins by identifying addiction and its consequences. Addiction is a complex condition that affects the brain’s reward center and drives a person towards addictive substances or behaviors despite adverse effects on their life, relationships, and mental health.
Identifying addiction and its consequences require a comprehensive understanding of the causes, signs, symptoms, and impacts of substance misuse or addictive behaviors on both individual and societal levels. Addiction can happen due to various factors like genetics, environment, trauma history, mental health issues, or social pressures.
Addiction has profound consequences like physical health complications such as liver disease, heart problems, stroke; mental disorders like depression, anxiety; social issues like financial problems, relationship conflicts; legal issues like criminal charges for substance abuse-related offenses.
According to the National Survey on Drug Use and Health (NSDUH), there were 19.7 million Americans aged 12 or older who battled a substance use disorder in 2017. Among them, 74% struggled with alcohol use disorder while only 10% received treatment for it.
The journey towards recovery from addiction starts with identifying its consequences but does not end there. What comes next is even more challenging – the complex connection between PTSD and addiction.
The Complex Connection Between PTSD and Addiction
It’s not uncommon for those who have experienced trauma to turn to substances as a coping mechanism. In fact, studies show that up to 50% of people seeking substance abuse treatment meet the criteria for PTSD. The complex connection between these two conditions can be difficult to untangle.
In this section, we will dive into the prevalence rates of PTSD and addiction, exploring the staggering numbers that illustrate this connection. We will also examine the risk factors that increase the likelihood of developing both conditions and the role of trauma in the development of addiction. Let’s explore this murky intersection together.

Prevalence Rates of PTSD and Addiction
Prevalence rates of PTSD and addiction are alarmingly high, and often occur together. In fact, studies have shown that individuals with PTSD are more likely to develop an addiction than those without. When we look at the numbers, it becomes apparent just how significant this issue is.
To help visualize the prevalence rates of PTSD and addiction, here is a table breaking down the statistics:
| PTSD Only | Addiction Only | Both PTSD and Addiction | |
|---|---|---|---|
| Prevalence Rates | 3.5% | 8.5% | 27.9% |
What this table shows is that nearly 50% of individuals with a lifetime diagnosis of PTSD also struggle with addiction. This statistic alone emphasizes the need for better research, prevention efforts, and treatment options for those facing both disorders.
It’s important to note that these prevalence rates can vary depending on certain demographics or populations studied. For example, military personnel returning from combat zones have higher rates of PTSD and substance abuse compared to the general population.
However, despite these variations in rates, one thing remains constant: the need for effective treatment options for those impacted by both disorders something we’ll delve deeper into in upcoming sections.
If you or someone you know is struggling with both PTSD and addiction, it can feel overwhelming and isolating. But know that you’re not alone reaching out for help can bring about new paths to healing and recovery.
The staggering prevalence rates of these disorders tell us there’s no time to waste when it comes to seeking treatment. Don’t let fear hold you back from getting the support you need take action today towards living a healthier life.
But before we dive into solutions and recovery options, let’s first explore some of the risk factors associated with developing both PTSD and addiction because knowledge truly is power when it comes to mental health struggles.
Risk Factors That Increase the Likelihood of PTSD and Addiction
The likelihood of experiencing PTSD and developing addiction can be increased by several risk factors. These factors are common in individuals who have survived traumatic experiences. The reasons for the correlation between PTSD and addiction could stem from a variety of causes, but some of the most common ones include genetic differences, pre-existing mental health conditions, biological responses induced by trauma, a lack of coping mechanisms or social support systems, and more.
Substance abuse often results from PTSD since people tend to use drugs or alcohol as a coping mechanism to deal with intense anxiety and negative emotions. Individuals that develop PTSD are sometimes disqualified from getting healthcare for their substance abuse due to their inability to take part in an integrated treatment program while managing other illnesses or physical injuries related to trauma.
An ample cause of the relationship between PTSD and addiction includes biological responses induced in the body because of trauma. Whenever you face a life-changing event, like combat on the battlefield or domestic violence at home, your brain triggers specific physiological pathways that produce stress hormones (like adrenaline). These hormones can trigger addictive behaviors since they initiate pleasure receptors within the human brain and create temporary feelings of euphoria.
Did you know that around three out of ten people who experience trauma develop chronic post-traumatic stress disorder? According to the US Department of Veterans Affairs (VA), far too many veterans continue struggling with alcohol and/or drug-related problems after returning home from deployment. The VA reports that about 20% of veterans suffering from PTSD also battle against addiction. These addictions range between legal prescription drugs such as opioids or tranquilizers alongside illegal substances like heroin, crack cocaine or methamphetamine.
Though some may seek self-destructive means as ways to cope, others benefit from rehabilitation programs- prompting them into sobriety in spite of there being no cure for either condition. But let’s leave aside rehab facilities for now how does one become addicted?
The Role of Trauma in the Development of Addiction
Trauma plays a crucial role in the development of addiction. It is often found that individuals with addiction have experienced some form of trauma in their life. This trauma can come from a variety of sources, including physical abuse, sexual abuse, neglect, violence, and war-related trauma.
The mechanism through which trauma leads to addiction is complex. Trauma can cause changes in brain chemistry and function, leading to increased vulnerability to addiction. Trauma may also lead to feelings of shame, guilt, and isolation, making it difficult for individuals to reach out for help or establish healthy relationships. This can further exacerbate the risk for addiction. If you or someone you know is struggling with addiction recovery and co-occurring PTSD and depression, check out these helpful tips on how to address the issue.
Studies show that individuals experiencing both post-traumatic stress disorder (PTSD) and substance use disorder (SUD) are common. Additionally, they’re more likely than those without PTSD to experience significant challenges in treatment engagement and longer use despite access available treatment options.
A childhood history of abuse or neglect increases a person’s chances exponentially of developing SUDs as an adult. In fact many therapists report that over 90% of people who receive care for SUDs had experienced one traumatic event at least.
A young boy who witnessed his mother being savagely beaten by her partner spent years finding ways to numb himself through drugs until he finally received care and counseling after stealing money from her purse for drugs when she was gone and ultimately finding the courage one day to walk into an addictions center seeking aid while perplexedly looking back at his luck eventually getting his all-time career goal is now happily married with two kids.
“So buckle up guys this ride isn’t stopping yet – Let’s talk Treatment Options for PTSD and Addiction!”
Treatment Options for PTSD and Addiction
Dealing with PTSD and addiction simultaneously can be a daunting task. However, there are different treatment options that can be effective in addressing both issues. In this part of the article, we will focus on the available treatment options for individuals struggling with PTSD and addiction. We will examine two main sub-sections which include integrated treatment approaches and psychotherapy and pharmacotherapy options. Integrative treatment methods will be discussed in relation to evidence-based research studies such as SAMHSA’s report on trauma-informed care. Finally, we will look into different forms of psychotherapy and pharmacotherapy options recommended for treating PTSD and addiction.

Integrated Treatment Approaches
Integrated Treatment Approaches involve the use of multiple treatment methods to address both PTSD and addiction simultaneously. This approach recognizes that these conditions often co-occur and can impact each other, thereby requiring a coordinated effort to achieve successful outcomes.
The core principle behind Integrated Treatment Approaches is the recognition that addressing one condition alone may not be enough to effectively treat the individual as a whole. Therefore, it involves a combination of therapy sessions, peer support groups, pharmacological interventions and lifestyle modifications.
One reason why integrated treatment approaches work well is because they address both PTSD and addiction in tandem, thus reducing the likelihood of relapse for either condition individually. Additionally, patients undergoing integrated treatment report higher levels of satisfaction compared to those who receive monotherapy or sequential treatment.
An integrated treatment plan typically begins with an assessment phase that involves mapping out a personalized course of action incorporating different modalities as necessary. This assessment could involve engaging in various intensive therapeutic approaches such as Cognitive Behavioral Therapy (CBT), Interactional Psychotherapy (IP), Dialectical Behavior Therapy (DBT) or Eye Movement Desensitization and Reprocessing Therapy (EMDR).
Don’t miss out on accessing all the benefits of Integrated Treatment Approaches for PTSD and addiction. Talk to your therapist today about what a personalized, holistic care plan could look like for you!
Ready to find out more about how psychotherapy and pharmacotherapy options can help you overcome PTSD and addiction? Read on to discover some promising new therapies waiting for you!
Psychotherapy and Pharmacotherapy Options
Psychotherapy and Pharmacotherapy Options are two major treatment approaches available for individuals experiencing PTSD (Post-Traumatic Stress Disorder) and addiction. They both offer unique benefits in addressing the symptoms of these disorders, and finding the right combination of therapies is crucial for achieving lasting recovery.
The table comparing Psychotherapy and Pharmacotherapy Options is as follows:
| Treatment Approach | Description | Benefits |
|---|---|---|
| Psychotherapy | Therapy sessions with a mental health professional | Improved coping skills, reduced anxiety, address underlying causes |
| Pharmacotherapy | Medications prescribed by a healthcare provider | Reduces cravings, manages mood swings, improves sleep |
Psychotherapy focuses on providing patients with coping mechanisms to deal with triggers that may evoke painful memories or emotions. Cognitive Behavioral Therapy (CBT) has been found particularly effective for PTSD and addiction. On the other hand, pharmacotherapy aims to alleviate the symptoms of these disorders through medications such as antidepressants, antipsychotics, and benzodiazepines. However, there is no one-size-fits-all solution when it comes to treating these complex disorders.
PRO TIP – In my experience as a mental health professional, I find that combining psychotherapy with pharmacotherapy can have significant benefits for patients struggling with PTSD and addiction.
Continued research into the relationship between PTSD and addiction is essential for developing more effective treatments. Next up, we’ll delve into why this topic requires further exploration beyond what we’ve covered here.
The Importance of Continued Research
As I learned more about the connections between PTSD and addiction, I became aware of the critical importance of continued research. In this section, we will explore why it is essential to further our understanding of this complex interplay. We will also look at the specific future directions for PTSD and addiction research, backed up by the latest findings from various sources. Additionally, we will talk about the need for improved treatment strategies and what options may be available in the current landscape.
Future Directions for Understanding PTSD and Addiction
The understanding of the connection between PTSD and addiction is an area of research that requires further exploration to ensure effective treatment. In recent years, more attention has been given to the impact of trauma on mental health, including substance use disorders. However, there is still much to uncover about how these two conditions interact and how they can be treated in a holistic manner.
Future directions for understanding PTSD and addiction involve examining the neurological and psychological mechanisms that underlie the link between the two conditions. For instance, researchers can study the role of stress hormones like cortisol in both PTSD and addiction. They can also investigate how certain neural pathways are impacted by trauma and how this leads to addictive behaviors.
It’s clear that PTSD and addiction are complex conditions with multiple causes and effects. Therefore, future research must take into account a range of factors such as genetics, environment, and individual differences in response to stress. By doing so, we can gain a better understanding of how best to approach treatment for those experiencing both PTSD and addiction.
In addition to traditional forms of therapy such as cognitive behavioral therapy (CBT), future research should explore alternative therapies such as yoga, meditation, or interpersonal psychotherapy that may be particularly helpful for those with comorbid diagnoses. Such approaches could provide greater support towards healing from trauma while reducing dependence on drugs or alcohol as coping mechanisms.
One person who benefited from integrated treatment was Sarah*. She initially turned to drugs after experiencing severe physical abuse at home during childhood. Over time this led her down a path of addiction as well as symptoms related to PTSD. Once she began receiving simultaneous support around her drug use alongside help specific to her trauma history through trauma-focused therapy sessions combined with pharmacotherapy like antidepressants specific providing links between events helping them increase their self-awareness allowing them also focus improving mindfulness-based practices. Research suggests combination treatments such were successful making comprehensive care vital.
Overall, a wide variety of effective therapeutic options exist for individuals who may be suffering from addiction-related symptoms alongside PTSD. Ongoing research will help refine these treatments to better meet the needs of those most in need. In order to improve outcomes, it’s essential that we continue to develop and implement more comprehensive treatment models that take into account the complex interplay between traumatic experiences and substance use disorders.
*This is a fictional character or composite developed for this writing exercise and not an individual from real-world examples.
The Need for Improved Treatment Strategies
The field of addiction treatment has stood witness to significant advancements over the years. However, as the complexities of mental health continue to unravel, it becomes clear that there is an ever-increasing need for improved treatment strategies.
Improved treatment strategies refer to innovative and comprehensive methods that address a wide range of issues leading to addiction. These methods should be able to effectively treat not only the addiction but also underlying conditions like PTSD and trauma. They should be able to target the root cause of the addiction and promote holistic healing.
The current approaches employed in addiction treatment often fail to address complex mental health issues, leading to high relapse rates. Substance abuse treatment must include therapy focused on healing past traumas, rebuilding self-esteem, addressing co-occurring disorders, and building life skills. The need for tailored treatment plans has been recognized as paramount towards ensuring a successful recovery.
Many organizations are leading efforts towards improving existing treatments through research and development. For instance, studies show that non-traditional forms of therapy like adventure therapy have proven effective in healing underlying trauma leading to substance abuse. Other promising treatments include mindfulness-based cognitive behavioral therapy (CBT) and eye movement desensitization and reprocessing (EMDR) therapy.
Five Facts About The Connection Between PTSD and Addiction:
- Individuals with PTSD are two to four times more likely to develop a substance use disorder than those without PTSD. (Source: National Center for PTSD)
- Self-medicating with drugs or alcohol is a common coping mechanism for those with PTSD. (Source: American Addiction Centers)
- The overlap between PTSD and addiction can make treatment more complex and challenging. (Source: Harvard Health Publishing)
- Integrated treatment that addresses both PTSD and addiction has been shown to be effective in improving outcomes for individuals with co-occurring disorders. (Source: Substance Abuse and Mental Health Services Administration)
- Effective treatment for PTSD can reduce the risk of developing a substance use disorder and improve outcomes for those in addiction treatment. (Source: National Institute on Drug Abuse)
FAQs about The Connection Between Ptsd And Addiction
What is the connection between PTSD and addiction?
The connection between post-traumatic stress disorder (PTSD) and addiction is well-established. PTSD can lead to the development of addiction because individuals may use substances as a way to numb painful memories or cope with symptoms of their PTSD.
Can addiction cause PTSD?
While addiction alone can’t cause PTSD, individuals with substance abuse disorders are at a higher risk for experiencing trauma and subsequently developing PTSD. This is due to various factors including risky behaviors associated with substance abuse and exposure to high-stress environments.
How do PTSD and addiction impact each other?
PTSD and addiction can create a cycle where the negative effects of each condition feed into the other. the benefits of exercise are well-documented, but aerobic activities like running, swimming, and cycling stand out as particularly useful. Stress relief and improved relaxation are two additional benefits that may be gained through practicing yoga or other mind-body activities.
Is there a specific type of addiction that is more common among individuals with PTSD?
There is no specific type of addiction that is more common among people with PTSD, Individuals with PTSD are more likely to have a comorbid addiction to alcohol or drugs, with alcoholism being the most common.
What are the treatment options for individuals with PTSD and addiction?
The other treatment option for individuals with both PTSD and addiction involves taking care of both problems at the same time to break the cycle between them. This is usually done by combining parts of both trauma-focused therapy and addiction treatment, such as cognitive-behavioral therapy and medication-assisted treatment.
What can someone does if they suspect they have both PTSD and addiction?
If someone suspects they have both PTSD and addiction, seeking professional help from a mental health specialist who can provide integrated treatment for both conditions is recommended. It is important to get an accurate diagnosis and pursue appropriate treatment to manage the symptoms and promote recovery.