Benzodiazepines, often termed ‘benzos’, are medications designed to depress the central nervous system, effectively reducing anxiety, aiding sleep, and preventing seizures. As they modulate the neurotransmitter GABA, what are benzodiazepines? They are powerful, but their usage must be carefully managed due to risks like dependency. This article unpacks the essential knowledge surrounding benzodiazepines, guiding you through their uses, effects, and safety precautions.
Key Takeaways
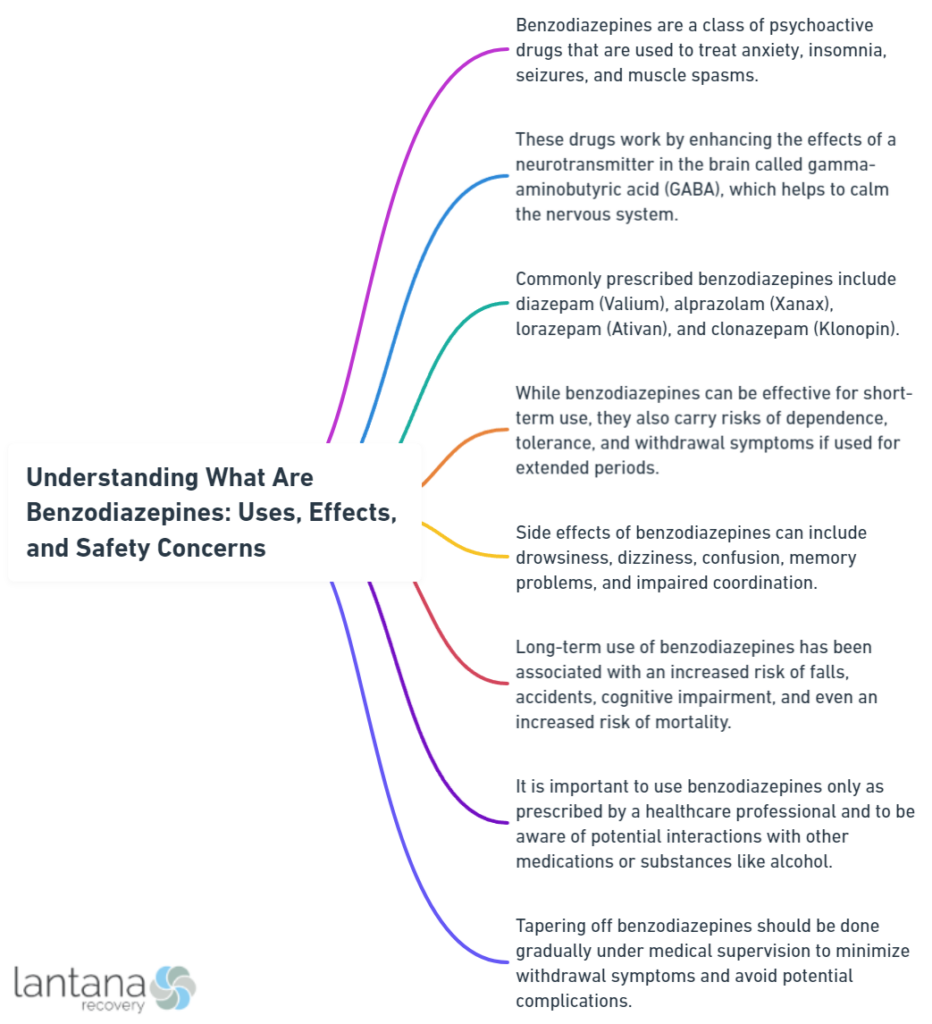
- Benzodiazepines are central nervous system depressants that augment the effects of the neurotransmitter GABA, inducing calm and relaxation, and are used to treat anxiety, insomnia, muscle spasms, and prevent seizures, but their effectiveness and duration vary due to differences in chemical structure.
- Despite their clinical benefits in treating anxiety and panic disorders, managing sleep disturbances, and aiding alcohol withdrawal, benzodiazepines carry significant risks, including cognitive impairment, dependence, and withdrawal symptoms, necessitating careful use and monitoring.
- Alternatives to benzodiazepines, such as cognitive-behavioral therapy, lifestyle changes, and various supplements, can provide safer long-term solutions for managing anxiety and sleep disorders, with healthcare providers encouraged to employ responsible prescribing, patient education, and monitoring practices.
Defining Benzodiazepines: A Pharmacological Overview

Benzodiazepines, often referred to as “benzos,” are medications that act as central nervous system (CNS) depressants. They slow down the messages traveling between the brain and the body, making the nervous system less active. This tranquilizing effect is achieved by enhancing the effect of the neurotransmitter gamma-aminobutyric acid (GABA). GABA is an inhibitory neurotransmitter, meaning it reduces neuron excitability, leading to calming effects. By enhancing GABA’s effect, benzodiazepines help to:
- Alleviate feelings of anxiety
- Induce sleep
- Relax muscles
- Prevent seizures
Having grasped the basics of benzodiazepines and their functioning, we’ll now dig deeper into the subject. You might be wondering, “If all benzodiazepines enhance GABA’s effect, why are there so many different types?” The answer lies in their unique chemical structures.
The Chemical Nature of Benzodiazepines
At the heart of every benzodiazepine is a core chemical structure consisting of a benzene ring fused to a seven-membered diazepine ring. What sets individual benzodiazepines apart are the variations in this chemical structure, specifically, different substitutions at specific positions on the benzene ring. These variations result in a diversity of pharmacological properties, which explains why different benzodiazepines can have varying effects and durations of action. Some common benzodiazepines include:
-
Alprazolam (Xanax)
-
Diazepam (Valium)
-
Lorazepam (Ativan)
-
Clonazepam (Klonopin)
-
Temazepam (Restoril)
It is important to note that taking benzodiazepines should only be done under the guidance of a healthcare professional, as they can be habit-forming and have potential side effects.
Benzodiazepines are often classified based on their duration of action into the following categories:
- Ultra-short-acting
- Short-acting
- Intermediate-acting
- Long-acting
This duration of action is influenced by factors such as the drug’s half-life and the presence of active metabolites. For instance, short-acting benzodiazepines are eliminated from the body fairly quickly and are often used for conditions like insomnia, where a rapid onset and offset of action is beneficial. On the other hand, longer-acting benzodiazepines, with their slower elimination, are useful for conditions like anxiety, where a sustained effect is desired.
Grasping the chemical nature of benzodiazepines provides a clearer picture of their internal functioning. Still, the real fascination with benzodiazepines is rooted in their interaction with the brain.
How Benzodiazepines Work in the Brain
Benzodiazepines work their magic by interacting with GABA receptors throughout the central nervous system. These receptors are like locks, and GABA is the key. When GABA binds to these receptors, it opens a channel allowing negatively charged chloride ions to enter the neuron. This makes the inside of the neuron more negative, making it less likely to fire and send a signal to other neurons. This results in the calming, sedative effect that benzodiazepines are known for.
But wait, where do benzodiazepines come into play? While benzodiazepines don’t unlock these doors themselves, they act like a VIP pass, making it easier for GABA to work its magic. Specifically, benzodiazepines:
-
Bind to a special site on the GABA-A receptors
-
Enhance the affinity of GABA for its receptor
-
Facilitate the opening of more chloride ion channels
-
Increase the inhibitory effect of GABA
-
Lead to greater sedation and muscle relaxation.
Benzodiazepines owe their potency to their ability to enhance GABA’s effect in the brain. However, this also underlines why their misuse or high-dose consumption can lead to significant side effects.
Having gained a comprehensive understanding of benzodiazepines’ molecular workings, we will now examine their clinical applications.
Clinical Uses of Benzodiazepines

Benzodiazepines are like a Swiss Army knife in the world of medicine – a single tool with multiple uses. They are often prescribed for a wide range of conditions, from anxiety and panic disorders to insomnia and even alcohol withdrawal syndrome. The reason for this versatility lies in the primary effect of benzodiazepines – their ability to calm the central nervous system.
Considering the prevalence of anxiety disorders and insomnia as mental health issues, the frequent use of benzodiazepines for their management is not unexpected. But how exactly do benzodiazepines help with these conditions?
Treating Anxiety and Panic Disorders
When it comes to managing anxiety and panic disorders, benzodiazepines have proven to be a reliable ally in the short term. They are highly effective in reducing the intensity of anxiety and panic attacks, providing temporary relief for individuals suffering from these debilitating conditions.
One benzodiazepine that’s particularly effective in this regard is alprazolam. Approved by the FDA for the treatment of both anxiety and panic disorders, including agoraphobia, alprazolam provides rapid relief by enhancing the inhibitory effects of GABA. Nonetheless, it’s crucial to bear in mind that benzodiazepines, such as alprazolam, are generally utilized as short-term solutions, given that prolonged use can result in dependence and other negative effects.
While benzodiazepines have been a mainstay in the treatment of anxiety and panic disorders, they also play a significant role in managing sleep disturbances, another common issue affecting mental health.
Managing Sleep Disturbances
Insomnia, characterized by difficulty falling asleep or staying asleep, is a common sleep disorder that can have a significant impact on quality of life. Benzodiazepines, with their sedative properties, have been used as a short-term solution for managing sleep disturbances like insomnia.
Several benzodiazepines are specifically approved for the short-term treatment of insomnia, including:
-
Doral (quazepam)
-
Dalmadorm/Dalmane (flurazepam)
-
Halcion (triazolam)
-
ProSom (estazolam)
-
Restoril (temazepam)
These medications, known as depressant drugs, work by enhancing the effect of GABA, promoting restful sleep by inducing a state of tranquility and relaxation.
While benzodiazepines might prove effective for managing sleep disturbances, they should not be viewed as a long-term solution. Long-term use of benzodiazepines can lead to dependence and other adverse effects, which we’ll delve into later. For now, let’s move on to another important clinical use of benzodiazepines: the management of alcohol withdrawal.
Benzodiazepines in Alcohol Withdrawal
Alcohol withdrawal syndrome is a potentially life-threatening condition that can occur when a person who has been drinking excessively suddenly stops or significantly reduces their alcohol intake. It’s in these scenarios that benzodiazepines, with their calming effects and ability to prevent seizures, have proven to be particularly valuable to treat alcohol withdrawal.
Chlordiazepoxide is a benzodiazepine that’s primarily indicated for managing alcohol withdrawal syndrome. Similarly, lorazepam, with its predictable intramuscular absorption, is effective in preventing the seizures associated with alcohol withdrawal. Long-acting benzodiazepines like chlordiazepoxide make the detoxification process more tolerable and reduce the risk of dangerous withdrawal effects.
As potent and versatile as benzodiazepines may be in treating various conditions, they are not without their risks. Let’s now turn our attention to the potential side effects and risks associated with benzodiazepine use.
Alcohol Rehab in South Carolina
Alcohol rehab in South Carolina offers individuals struggling with alcohol addiction a path towards recovery within a supportive and understanding environment. These facilities are equipped with specialized programs tailored to address the unique needs of each individual, ensuring comprehensive care and attention. Through a combination of therapy, counseling, and medical support, individuals can embark on a journey towards sobriety and long-term wellness. South Carolina’s alcohol rehab centers strive to provide a holistic approach to treatment, addressing not only the physical aspects of addiction but also the underlying emotional and psychological factors contributing to substance abuse. With a focus on personalized care and evidence-based practices, these facilities aim to empower individuals to overcome addiction and build a healthier, substance-free life.
Risks and Side Effects Associated with Benzodiazepine Use

While benzodiazepines can be highly effective in managing a range of conditions, they also come with a host of potential side effects and risks. These range from cognitive impairments, such as interference with memory formation, to physical dependence and withdrawal symptoms.
Prolonged benzodiazepine use can adversely affect all cognitive areas, most notably:
-
Visuospatial memory
-
IQ
-
Visiomotor coordination
-
Information processing
-
Verbal learning
-
Concentration
These cognitive impairments, coupled with the physical dependence that can develop with chronic use, make benzodiazepine use a double-edged sword.
How can we identify if someone is suffering from the adverse effects of benzodiazepine use?
Recognizing Adverse Effects
Benzodiazepines can cause a range of adverse effects, many of which are related to their action on the central nervous system. These include:
-
Drowsiness
-
Confusion
-
Dizziness
-
Difficulty thinking or reasoning
-
Euphoria
In essence, these effects are an over-amplification of the calming effect that benzodiazepines are intended to provide.
In addition to these central nervous system effects, benzodiazepines can also cause the following side effects:
-
Visual disturbances such as double vision and difficulty focusing
-
Gastrointestinal issues like nausea and vomiting
-
Respiratory symptoms like respiratory depression
-
Neurological symptoms such as headache, tremors, and fainting
While these adverse effects can be concerning, perhaps one of the most significant risks associated with benzodiazepine use is the potential for dependence and withdrawal symptoms.
Understanding Dependence and Withdrawal Symptoms
Benzodiazepines, especially when used long-term, can lead to the development of physical dependence. This means that the body adjusts to the presence of the drug, and withdrawal symptoms can occur when the drug is abruptly stopped or reduced. Withdrawal symptoms may manifest as:
-
Insomnia
-
Gastric problems
-
Tremors
-
Agitation
-
Fearfulness
-
Muscle spasms
These symptoms can be challenging to manage during the recovery process. In severe cases, seizures can occur during benzodiazepine withdrawal.
Individuals with a history of substance use disorders, such as those involving alcohol or drugs, are at a higher risk and should avoid using benzodiazepines to prevent dependence. Recognition of the risk of dependence on benzodiazepines became more evident in the 1980s, after initial optimism about their safety.
The protracted withdrawal syndrome from benzodiazepines can persist for many months, or in some cases, a year or longer. To manage benzodiazepine misuse and facilitate withdrawal, substituting short half-life benzodiazepines with longer half-life ones, such as diazepam, is a common strategy.
While understanding these risks is crucial, it’s equally important to be aware of the potential interactions and contraindications of benzodiazepine use.
What Are Schedule 8 Drugs
“What are schedule 8 drugs” refers to substances classified under Schedule 8 of the Standard for the Uniform Scheduling of Medicines and Poisons (SUSMP) in Australia. Schedule 8 drugs are those deemed to have a high potential for abuse or addiction, as well as severe health risks. They are tightly regulated due to their potential for harm and misuse. Examples of Schedule 8 drugs include strong opioids such as morphine, oxycodone, and fentanyl, as well as certain stimulants and sedatives. Prescriptions for these drugs typically come with stringent monitoring and prescribing requirements to mitigate risks associated with their use. Understanding the classification and regulations surrounding Schedule 8 drugs is crucial for healthcare professionals and individuals alike to ensure safe and responsible use.
Interactions and Contraindications

One of the challenges with benzodiazepines, as with many medications, is that they can interact with other substances, leading to potentially dangerous effects. Combining benzodiazepines with alcohol or opiates, for instance, can result in breathing difficulties and significantly increase the risk of overdose and death.
Benzodiazepines can be categorized into two groups based on their metabolism: those metabolized by cytochrome P450 enzymes, which have a higher potential for drug interactions, and those metabolized through glucuronidation, which have minimal drug interactions. The concomitant use of benzodiazepines with certain pharmaceutical drugs can lead to adverse effects such as breathing difficulties, exacerbating the risk of overdose and possible fatality. Therefore, careful monitoring of benzodiazepine use by healthcare providers is essential to prevent potentially harmful drug interactions.
But what happens when the body accumulates too much of a benzodiazepine due to these interactions?
Drug Accumulation and Interactions
Excessive accumulation of benzodiazepines in the body can occur if they are mixed with other drugs, leading to a dangerous benzodiazepine overdose. Some benzodiazepines, such as:
-
alprazolam
-
triazolam
-
brotizolam
-
midazolam
Controlled substances are primarily metabolized by the cytochrome P450 (CYP) 3A4 enzyme system.
Certain substances, including azole antifungals, macrolide antibiotics, calcium antagonists, and grapefruit juice, can inhibit the activity of CYP3A4. This inhibition can lead to increased levels of benzodiazepines in the body, potentially leading to an overdose. On the flip side, substances that induce CYP3A4 activity, such as antiepileptic drugs and rifampicin, can decrease benzodiazepine levels, reducing their effectiveness.
While understanding the potential for drug accumulation and interactions is vital, it’s equally important to know when not to use benzodiazepines.
When Not to Use Benzodiazepines
Benzodiazepines are powerful drugs, but they’re not suitable for everyone. For instance, people with advanced liver or kidney disease are advised against the use of benzodiazepines due to the risk of drug accumulation and toxicity. Pregnant or breastfeeding women should also avoid benzodiazepines due to the potential harm to the fetus or infant. Elderly individuals should use benzodiazepines with caution due to an increased risk of falls and subsequent injuries.
Additionally, individuals with respiratory conditions like acute asthma, emphysema, or sleep apnea should avoid benzodiazepines due to the risk of respiratory depression. Given the potential risks and side effects associated with benzodiazepines, it’s crucial that these medications are used responsibly.
Approaching Benzodiazepine Treatment Responsibly
Responsible use of benzodiazepines entails more than merely adhering to the prescribed dosage. It also includes adhering to prescribing guidelines, monitoring for misuse, and providing patient education on the risks and potential alternatives. Healthcare providers play a crucial role in this process. They should ensure a thorough patient history and evaluation for potential abuse or misuse of benzodiazepines before prescribing them. Regular monitoring of patients is also critical to identify any signs of benzodiazepine misuse, such as requests for early refills, multiple prescriptions, and escalating doses without guidance. Healthcare providers should also be cautious of the development of tolerance, physical dependence, and potential for withdrawal symptoms when patients use benzodiazepines.
What protocol should healthcare providers adhere to when prescribing benzodiazepines, especially when it comes to patients who have been prescribed benzodiazepines in the past?
Prescribing Guidelines
When it comes to prescribing benzodiazepines, guidelines recommend short-term use (ideally less than 2-4 weeks) to prevent tolerance and dependence. This is especially important in the management of severe anxiety or panic disorder, where benzodiazepines are often used in acute crisis situations.
When prescribing long-term benzodiazepines, healthcare providers should ensure adequate patient education on the risks and secure documentation of informed consent. Patients should be informed about the negative effects and benefits of discontinuing the drugs. The use of benzodiazepines in individuals 65 years or younger is associated with an increase in all-cause mortality. Therefore, a gradual reduction regimen is the recommended approach for reducing benzodiazepine dosage to minimize withdrawal symptoms.
Despite adhering to the best prescribing practices, the possibility of benzodiazepine misuse persists.
Monitoring for Benzodiazepine Misuse
Monitoring for benzodiazepine misuse is an essential part of safe and effective treatment. Here are some tools that can help:
-
Prescription drug monitoring programs can detect ‘doctor shopping’ and other forms of misuse among patients using benzodiazepines.
-
The Severity Dependence Scale (SDS) can provide a standardized assessment of benzodiazepine dependence.
-
Path2Help can provide tailored support information and services for individuals suspected of misuse.
Healthcare providers should be vigilant for signs of benzodiazepine misuse, such as double dosing or illicit selling, as they could indicate dependence or abuse. When it comes to managing benzodiazepine misuse and facilitating withdrawal, a gradual dose reduction strategy is often employed, sometimes utilizing a switch to a longer-acting benzodiazepine like diazepam.
Patients undergoing benzodiazepine withdrawal or therapy should have access to emotional or psychological support to aid in coping and managing underlying conditions. Utilizing motivational interviewing, staged dispensing, and considering specialist addiction services can be essential in managing benzodiazepine dependency and therapy for high-risk patients. Group practices should adopt a unified policy on benzodiazepine prescribing to ensure consistency and help resist patient pressures for prescriptions. Urine drug screening is a method to monitor for benzodiazepine use, although interpretation of results can be complex due to metabolite presence.
Benzodiazepines, while effective in managing a variety of conditions, are not the only treatment option available. Let’s explore some alternatives.
Who Can Prescribe Methadone
In many countries, regulations stipulate specific qualifications and licenses for individuals who can prescribe methadone. Generally, these regulations aim to ensure that only qualified healthcare professionals are authorized to prescribe this medication due to its potential for misuse and addiction. Typically, doctors, specifically those specialized in addiction medicine or pain management, can prescribe methadone as part of a comprehensive treatment plan for opioid dependence or chronic pain management. Additionally, some countries allow nurse practitioners and physician assistants, under certain circumstances, to prescribe methadone within their scope of practice. However, strict monitoring and adherence to regulations are crucial to prevent misuse and diversion of this potent medication. Collaboration among healthcare providers, including pharmacists and counselors, is often essential in ensuring safe and effective methadone therapy for patients.
Alternatives to Benzodiazepines
While benzodiazepines can be an effective treatment option for certain conditions, they are not the only solution. In fact, there are a number of alternatives to benzodiazepines that can offer relief without the associated risks.
Cognitive-behavioral therapy (CBT) is a recommended non-pharmacological therapy for anxiety and insomnia, often providing safer and more long-lasting results than benzodiazepine use. CBT works by helping individuals understand and change thought patterns leading to harmful behaviors or distressing feelings.
In addition to CBT, other alternative therapies such as acupuncture, massage, and a range of supplements including Passiflora, Kava, and CBD may offer relief for fatigue poor concentration anxiety and aid sleep. Lifestyle changes such as reducing caffeine, practicing relaxation techniques, and dietary adjustments including consumption of fermented foods and avoidance of certain additives may also alleviate anxiety symptoms.
Furthermore, environmental medicine, including the reduction of heavy metal bioaccumulation, and the consumption of magnesium-rich foods can support mental health without depending on benzodiazepines.
Summary
Benzodiazepines, with their potency and versatility, have been a mainstay in the treatment of various conditions such as anxiety, panic disorders, insomnia, and alcohol withdrawal syndrome. However, their use is not without risks, including side effects, dependence, and withdrawal symptoms. Responsible use involves adhering to prescribing guidelines, monitoring for misuse, and exploring alternatives when possible. As we continue to navigate the complex world of benzodiazepines, it’s crucial that we balance their therapeutic benefits with their potential risks, always striving for the safest and most effective treatment outcomes.
Frequently Asked Questions
What are examples of benzodiazepines?
Examples of benzodiazepines include Alprazolam (Xanax), Clonazepam (Klonopin), Lorazepam (Ativan), and Diazepam (Valium). These are commonly used as anxiolytics and sedatives.
What benzodiazepines do to your body?
Benzodiazepines slow down the messages between the brain and the body, treating symptoms of anxiety or insomnia but not the underlying causes. They are central nervous system depressants and can cause drowsiness, lethargy, impaired motor coordination, and other side effects.
What is the problem with benzodiazepines?
The problem with benzodiazepines includes irritation, personality changes, weakness, drowsiness, and lack of motivation. These adverse effects can significantly impact the individual’s well-being.
Are benzodiazepines antidepressants?
Benzodiazepines are not antidepressants; they are a group of depressant drugs primarily prescribed for anxiety, sleeping problems, and other symptoms unrelated to depression. It is important to use them only as prescribed.
What are benzodiazepines used for?
Benzodiazepines are used to treat various conditions such as anxiety disorders, panic disorder, sleep disorders, and alcohol withdrawal syndrome. They are prescribed for a wide range of medical issues.