Key Takeaway:
- Co-occurring PTSD and depression are complex conditions and must be addressed concurrently in addiction recovery. Understanding the key differences and similarities, recognizing symptoms, and learning about the causes are crucial steps in effectively addressing co-occurring conditions.
- Co-occurring PTSD and depression can pose significant challenges for addiction recovery, and traditional treatment approaches may not be sufficient. Overcoming barriers to treatment and developing a comprehensive and individualized treatment plan is key to success.
- Effective treatment for co-occurring PTSD and depression in addiction recovery may include talk therapies, medication, and alternative therapies. Additionally, practicing self-care strategies and developing a strong support system are important for both short and long-term management of these conditions.
Are you struggling with addiction, depression and PTSD? You’re not alone. This article explores practical ways to effectively and holistically address this often difficult and complex situation. With the help of evidence-based practices, you can start your journey to healing and recovery.
Understanding Co-occurring PTSD and Depression
As someone who’s struggled with addiction myself, I know all too well the impact that co-occurring mental health disorders can have on the recovery process. In this part of the article, we’ll dive into the complexities of addressing co-occurring PTSD and depression in addiction recovery. We’ll start by exploring the differences and similarities between these two mental health disorders, so that we can better understand how they can both impact addiction. Then, we’ll take a closer look at the symptoms of co-occurring PTSD and depression, as well as some of the underlying causes that can contribute to their development.

Defining PTSD and Depression: Key Differences and Similarities
Defining PTSD and Depression: Key Differences and Similarities can be confusing for some individuals. Both conditions are mental health disorders but they have their own unique characteristics. It is important to understand their differences and similarities to properly address them.
To better understand the key differences and similarities between PTSD and depression, a HTML table has been created. The first column lists down the characteristics of PTSD while the second column lists down the characteristics of depression. The third column highlights whether those characteristics are similar in both disorders or different from each other.
| PTSD Characteristics | Depression Characteristics | Similar or Different |
|---|---|---|
| Re-experiencing a traumatic event through flashbacks, nightmares, or intrusive thoughts | Feelings of sadness, hopelessness or worthlessness | Different |
| Difficulty concentrating | Difficulty concentrating | Similar |
| Emotional numbness and avoidance | Loss of interest in activities | Different |
| Hypervigilance and irritability | Change in appetite and weight | Different |
| Unique to PTSD: | Unique to depression: | |
| Flashbacks | Suicidal thoughts | Different |
In terms of symptoms, PTSD focuses on re-experiencing a traumatic event through flashbacks, nightmares, or intrusive thoughts while depression centers on feelings of sadness, hopelessness or worthlessness. However, difficulty concentrating is a similarity between these two conditions which can lead to issues with daily activities like work or school.
Complex trauma often leads to both PTSD and depression for many individuals as both disorders are linked to emotional regulation issues. However, while flashbacks are unique to PTSD, suicidal thoughts may accompany depression more often than not. The key difference between these two conditions though remains in their treatment techniques.
Pro Tip: Without proper psychological consultation it’s best to avoid self-diagnosing any mental disorders as misinterpreting your diagnosis can become counter-productive.
Recognizing the Symptoms of Co-occurring PTSD and Depression crafted from recognition (root word) we may further classify as ‘How do I recognize my own symptoms?’ Identifying co-occurring PTSD and Depression at early stages will help improve recovery rates eliminating any underlying addiction risks that arise from self-medicating practices one partakes due to undiagnosed bouts of anxiety/depression.
Overall untreated co-occurring conditions pose a high risk when one is navigating addiction recovery programs so it s crucial for clinicians and clients alike to recognize its presence at an earlier stage instead of brushing it off altogether without prioritizing it in therapy sessions.
Recognizing the Symptoms of Co-occurring PTSD and Depression
Recognizing the Symptoms of Co-occurring PTSD and Depression can be a challenging task. These mental health conditions often appear in tandem, making diagnosis complicated. However, understanding subtle nuances between them is crucial since both contribute to substance abuse addiction, and addressing them with primary intervention could lead to successful recovery.
Symptoms of depersonalization, a wave of negative feelings, despair, intrusive thoughts and memories are characteristic for PTSD – Post-Traumatic Stress Disorder. In contrast, Depression manifests itself in numbness, loss of interest in life’s activities coupled with fatigue, insomnia or hypersomnia. Together they make individual struggles even more complex.
If you or someone you know is struggling with addiction and also experiencing symptoms of PTSD and/or depression, it is important to understand the connection between PTSD and addiction. This can help in addressing the co-occurring conditions and promoting effective addiction recovery.
One interesting factor about PTSD and Depression is that not everyone who experienced trauma develops it; therefore early recognition is essential when they do start showing signs. Instead of being the outcome of psychological stressors as perceived by popular belief on the surface level, they occur due to changes in brain structure associated with traumatizing experiences.
Pro Tip: If you suspect that someone close to you may have PTSD and Depression address it cautiously instead of brushing it off or pointing it out harshly – caring attitude makes all the difference.
Understanding reasons behind co-occurrence requires exploring them further via a similar physiological perspective and environment one observes towards substance use disorder related addiction establishment pathways.
Understanding the Causes of Co-occurring PTSD and Depression
Understanding the causes of co-occurring PTSD and depression is crucial to address them in addiction recovery. Often, individuals with addiction struggle with both PTSD and depression simultaneously, leading to more complicated treatment processes. Ignoring one condition can worsen the other, making it necessary to treat them together.
PTSD and depression have a reciprocal relationship, meaning they can cause, worsen, or trigger each other. For example, if someone experiences trauma that leads to PTSD, they might start feeling hopeless, fatigued or lose interest – all common symptoms of depression. Similarly, if someone has been living with depression and has a traumatic experience (“trigger”), it can develop into PTSD.
Research suggests that there’s no single cause of co-occurring PTSD and depression as it can result from various biological, environmental as well as psychological factors. Genetics play an essential role in shaping how an individual responds to stressors. Exposure to long-term stressors (e.g., abusive childhood experiences) or cumulative trauma exposure (e.g., war veterans) increases the likelihood of developing both conditions.
An alarming statistic shows that around 50% of those who seek treatment for substance use disorders (SUDs) globally have co-occurring mental illnesses like PTSD and Depression. However disheartening these numbers may seem at first glance; it’s important to note that recovery is possible for those experiencing both diagnoses.
One individual I worked with suffered from anxiety since early childhood due to ongoing domestic abuse from alcoholic parents; they joined a support group after experiencing triggers that caused flashbacks during drug addiction treatment sessions. They found relief meeting others who could relate and went on to complete rehab successfully while regularly attending self-help meetings.
As I wrapped up their session last week, I realized addressing these issues requires exploration without shame or judgment necessary for successful recovery for any affected individuals be they myself or anyone else trying bravely attempting this journey towards better mental health.
The Impact of Co-occurring PTSD and Depression in Addiction Recovery
In addiction recovery, co-occurring post-traumatic stress disorder (PTSD) and depression can pose a significant challenge. Dealing with one of these mental health disorders is hard enough, but navigating both of them at the same time can seem like an impossible feat.
So, how can we address these co-occurring conditions in addiction recovery? In this section, we ll explore:
- The impact that PTSD and depression can have on addiction recovery
- The challenges of recognizing and treating co-occurring PTSD and depression in recovery
- Provide insights into developing an effective treatment plan
Let s dive in and explore this complex issue.
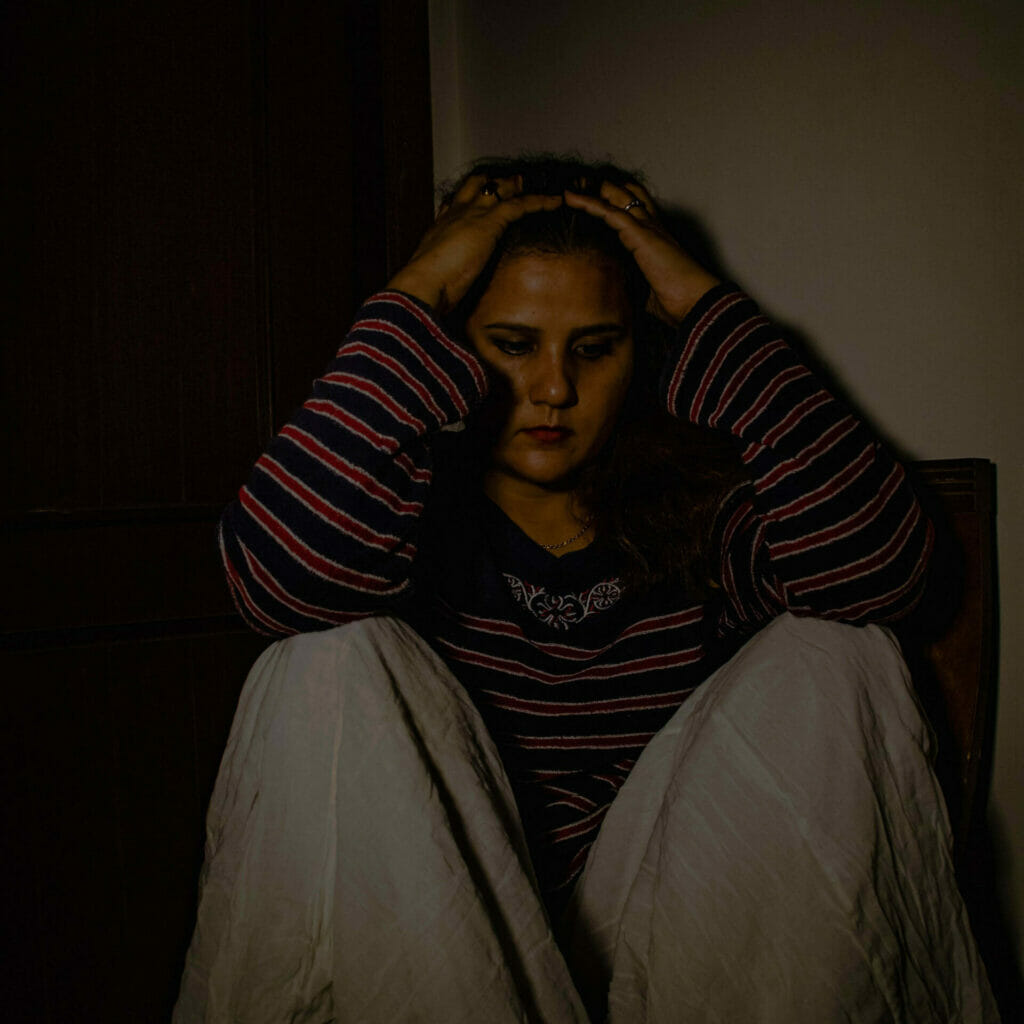
Recognizing the Challenging Nature of Co-occurring PTSD and Depression
Recognizing the challenging nature of co-occurring PTSD and depression is vital in addiction recovery as these two conditions often have a complex interplay that can significantly impact a person’s mental health. Understanding how they work together can help address their effects on people who are struggling with substance abuse and co-occurring mental health disorders.
PTSD, or post-traumatic stress disorder, is a mental health condition that affects individuals who have experienced, witnessed, or been confronted with traumatic events such as sexual assault, physical violence, accidents, or natural disasters. Depression, on the other hand, is a persistent feeling of sadness, low mood, and hopelessness that lasts for weeks to months. While both of them are different disorders, they can occur together and lead to more severe symptoms than either condition alone.
Recognizing the challenging nature of co-occurring PTSD and depression is essential because of how they feed into each other. Depression exacerbates negative thoughts and emotions associated with PTSD while further increasing feelings of isolation and hopelessness caused by the trauma. Similarly, untreated PTSD symptoms contribute to worsening depressive symptoms such as social isolation and decreased pleasure. Thus it creates a vicious cycle that needs proper attention to break.
Interestingly enough since depression evolves differently in people with PTSD leads to chronicity much quicker than those affected by either issue; engagement for accurate studies must be partaken through various background datasets. It will prove valuable for treatment models not limited to substance misuse recovery facilities but from general practitioners also.
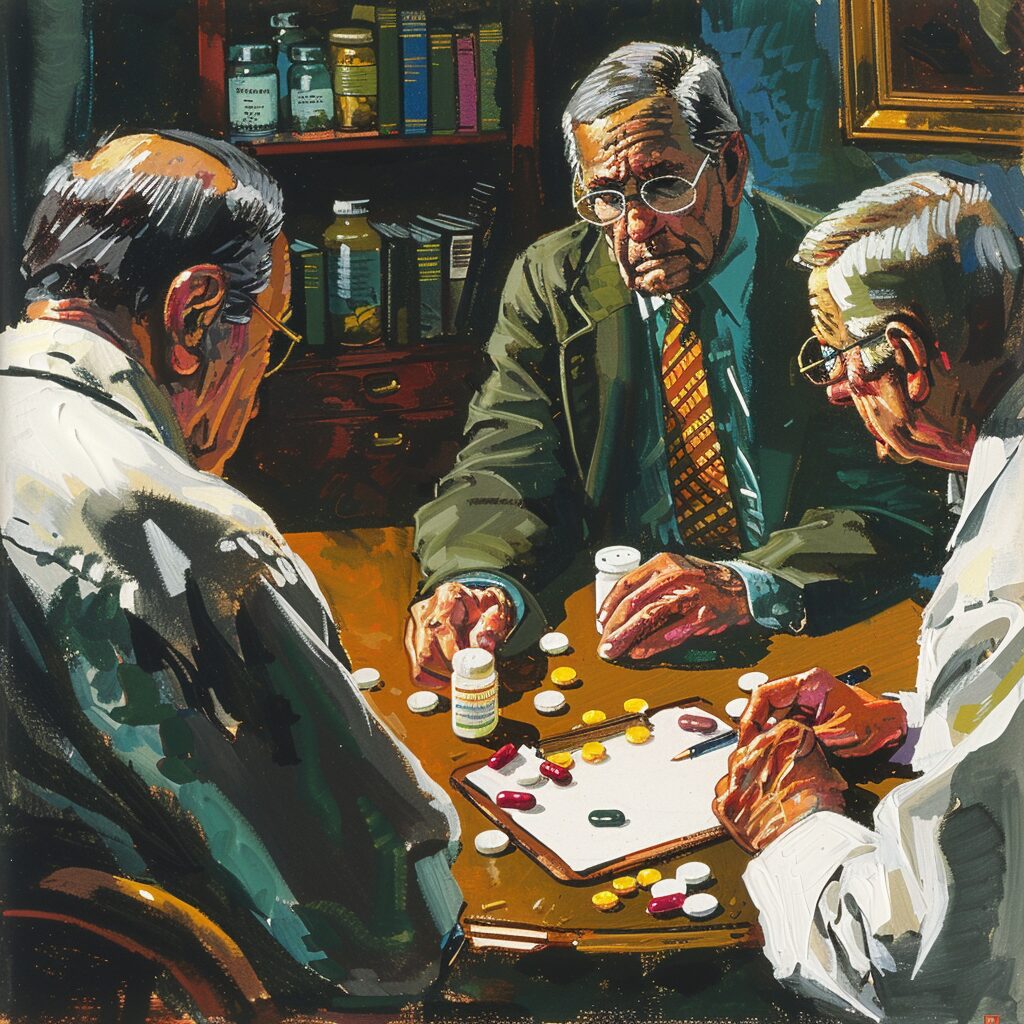
Notably recorded dialogues between senior doctors indicate that John (alias) was “paranoid” they suggest he should have seen an increase in medication which constricts recovery options as there isn’t access to complementary therapies helping guide patients who may not show improvement through traditional medications.
Now let’s tune ourselves into discovering ‘Understanding Barriers To Treating Co-occurring PTSD And Depression In Recovery’ in identifying possible solutions any patient has with coping mechanism techniques.
Understanding Barriers to Treating Co-occurring PTSD and Depression in Recovery
Understanding Barriers to Treating Co-occurring PTSD and Depression in Recovery is crucial for addiction treatment. In order to address these co-occurring disorders successfully, it is necessary to first comprehend the challenges that come with treating them.
People who struggle with addiction often have underlying mental health issues such as PTSD and depression. These mental illnesses can be hindrances to addiction recovery due to their unique sets of barriers. For instance, individuals who have both PTSD and depression may experience intense emotions, chronic anxiety, feelings of hopelessness, social isolation, and other symptoms that make recovery challenging. Factors like shame around asking for help, limited access to resources or stigma surrounding mental health further compound these impediments.
Additionally, treating individuals with co-occurring PTSD and depression requires specialized knowledge and resources on the part of healthcare providers. Sometimes therapeutic interventions from individual counseling sessions are not enough. Patients may need pharmacological intervention or more intensive levels of care such as a residential rehab program.
Understanding Barriers to Treating Co-occurring PTSD and Depression in Recovery involves being aware of the issues that arise from socialization problems and difficulty communicating thoughts to other people. It also involves knowing how underlying trauma has an effect on recovery outcomes.
Research into effective treatments for co-occurring disorders supports the idea that comprehensive care plans are best suited for those seeking long term recovery success. This understanding creates an urgency among us all; if not equipped with enough information about these barriers then we run the risk of never fully comprehending how critical this issue is in addiction recovery.
Don’t let lack of understanding be your excuse for failing someone trying to beat addiction; read on about Developing an Effective Treatment Plan for Co-occurring PTSD and Depression in Recovery using insights from our experts!
Developing an Effective Treatment Plan for Co-occurring PTSD and Depression
Developing an Effective Treatment Plan for Co-occurring PTSD and Depression is crucial in addiction recovery, as these two conditions often go hand-in-hand. PTSD or post-traumatic stress disorder, and depression both require attention to ensure a successful recovery from addiction. Developing the right treatment plan requires a thorough understanding of each individual’s needs.
A treatment plan for co-occurring PTSD and depression is designed to address both conditions simultaneously. The goal is to provide patients with the support they need as they work through their addiction with the added pressure of managing these mental health conditions. This approach can be effective because it acknowledges that treating one condition may not be enough. Both PTSD and depression can impact an individual’s emotional, physical, and social well-being; therefore, addressing them simultaneously leads to improved outcomes.
Developing an Effective Treatment Plan for Co-occurring PTSD and Depression should include a range of evidence-based therapies tailored to each patient’s specific needs. There are many factors involved in developing such a plan, including family dynamics, trauma history, addiction severity, and mental illness diagnosis. Some of the treatments used may include behavioral therapy, cognitive processing therapy (CPT), psychoeducation sessions, or medication.
It is essential that patients fully participate in the development of their treatment plans by providing input on what has worked for them in the past and what they expect from treatment going forward. Reflection on their experiences can be as helpful as feedback on new strategies from therapists.
I once met a person who struggled with co-occurring PTSD and depression during her journey towards addiction recovery. She was so overwhelmed that she felt like giving up sometimes but being conscientious about her treatment plans helped her stay more focused throughout the process.
If you’ve been battling co-occurring PTSD and depression while also struggling with addiction, don’t worry – there are many effective treatments available to help you overcome those obstacles in the way towards recovery.
Ready for more? Buckle up as we delve into your treatment options for co-occurring PTSD and depression.
Treatment Options for Co-occurring PTSD and Depression
As someone who has personally experienced the challenges of addiction recovery, I know firsthand how difficult it can be to overcome the co-occurring issues of PTSD and depression. It s a complex issue that requires a multifaceted approach, and that s where treatment options come in.
In this section, we ll take a closer look at some of the most effective treatment options for co-occurring PTSD and depression. We will explore various talk therapy options, medication options, and alternative therapies, providing insight into each to help you make the best decision for your recovery.

Talk Therapy Options for Co-occurring PTSD and Depression
Talk Therapy Options for Co-occurring PTSD and Depression are gaining popularity in the field of addiction recovery. These therapies involve discussing past traumas, negative emotions, and cognitions with a therapist. Clients can expect to share their thoughts and feelings with an experienced listener who will help them manage these experiences through self-reflection, mindfulness training, exposure therapy, and cognitive-behavioral techniques.
Talk Therapy works well because it helps clients process their traumatic events while receiving empathy and validation from a trained therapist. Clients can expect to feel heard and understood by someone who genuinely cares about their well-being. Moreover, putting meaning to past traumas is beneficial for reducing symptoms of depression as well as resolving PTSD symptoms.
One valuable talk therapy option is Cognitive Processing therapy (CPT), which has been proven effective in treating co-occurring depression and PTSD. CPT teaches patients how to identify negative thoughts related to their trauma and replace them with positive ones. Additionally, Dialectical Behavioral Therapy (DBT) equips individuals with skills for living in the present moment through mindfulness training that can help manage both anxiety symptoms associated with PTSD as well as mood disorders like depression.
If you’re seeking Talk Therapy options for co-occurring PTSD and Depression, consider asking your therapist about Eye Movement Desensitization Reprocessing (EMDR). EMDR is an innovative treatment that contrasts traditional talk therapy interventions by incorporating rapid eye movements during sessions. The technique has been effective at reducing intrusive memories by changing how they’re stored in the brain’s memory system.
Next up: Medication Options for Co-occurring PTSD and Depression in Recovery – But before we jump into that, let’s take a deep breath, relax our shoulders away from our ears (yes…do it right now!), and use any form of anxiety relief tool that works best for us to help manage any heightened or unexpected reactions we may experience while reading on.
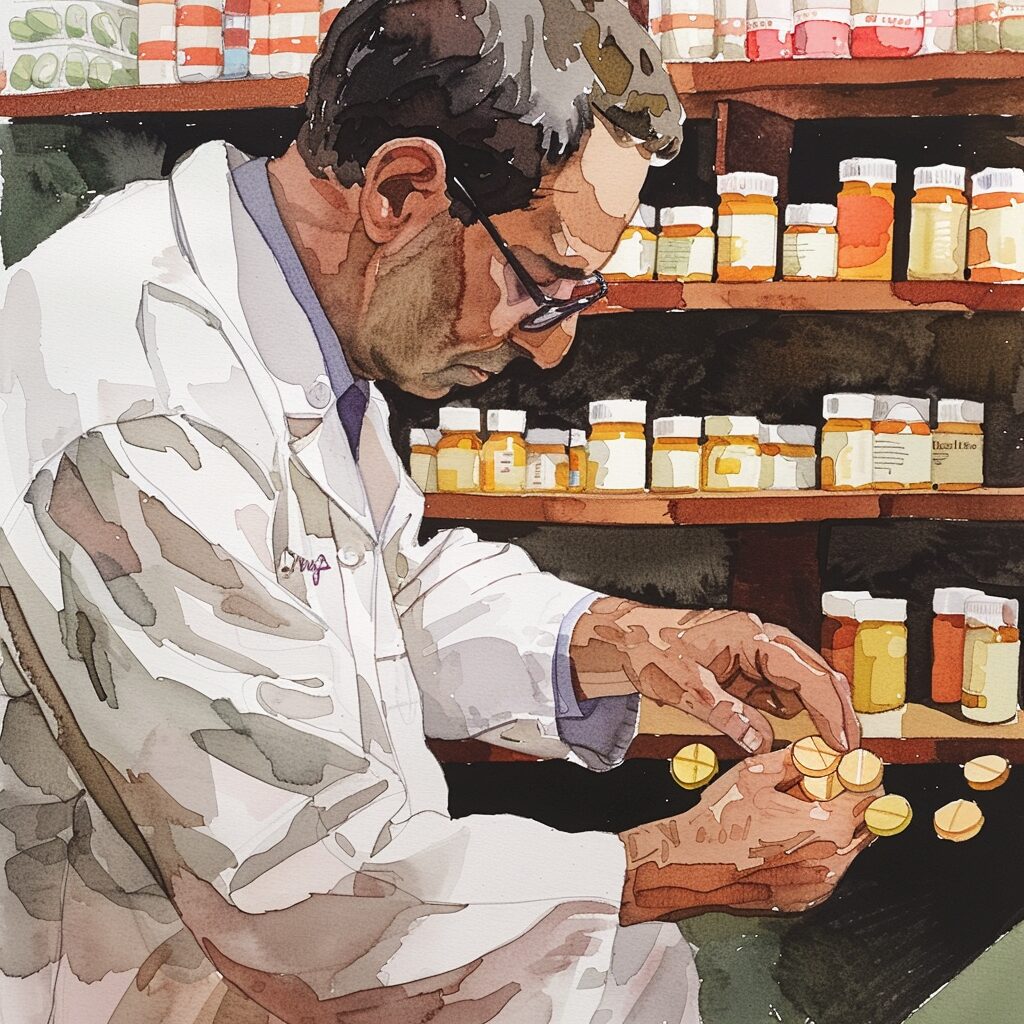
Medication Options for Co-occurring PTSD and Depression in Recovery
Medication Options for Co-occurring PTSD and Depression in Recovery
When it comes to treating co-occurring PTSD and depression in addiction recovery, medication can be an effective option to consider. Medication can effectively target specific symptoms of PTSD and depression, such as anxiety or insomnia, helping individuals feel more stable and focused on their recovery.
Medication works by targeting the chemical imbalances in the brain that are associated with PTSD and depression. For example, antidepressants can increase levels of serotonin in the brain, a chemical that regulates mood, while anti-anxiety medications can help manage symptoms of fear and anxiety.
It’s important to note that medication should never be the sole treatment approach for co-occurring PTSD and depression. Along with medication, therapy and support groups should also be a part of an individual’s overall treatment plan. Especially when dealing with addiction recovery – where emotional management is crucial – therapy can help individuals develop coping skills they need to manage symptoms long-term.
One valuable aspect of medication-assisted treatment (MAT) for co-occurring PTSD and depression is that it doesn’t have significant side effects when monitored properly by a healthcare provider. There is a risk of dependence for some medications used in MAT; however, when taken under clinical supervision, this risk is minimized.
If you or a loved one are struggling with co-occurring PTSD and depression in addiction recovery, don’t hesitate to speak with your healthcare provider about all the options available to you.
Don’t let fear hold you back from exploring all potential avenues of recovery. With the right treatment plan – which might include medication – many people living with co-occurring disorders find significant relief from their symptoms.
Ready to explore alternative therapies for addressing co-occurring PTSD and depression? Let’s dive into some other ways these conditions can be managed alongside addiction recovery.
Alternative Therapies for Co-occurring PTSD and Depression
Living with PTSD and depression can be a nightmare that never ends. Traditional therapies might not work effectively for everyone due to the co-occurring nature of these disorders. Alternative therapies are becoming increasingly popular in treating such conditions.
Alternative therapies are known to work by focusing on the body’s natural healing mechanisms, which is a stark contrast to traditional therapy, where medication and talk therapy are primarily used. Among the numerous alternative treatments available, Yoga and Meditation is an excellent choice for people struggling with Co-occurring PTSD and Depression. Yoga helps individuals connect with their mind, body, and spirit while seeking release from the constant bombardment of anxiety-provoking thoughts.
Furthermore, Emotional Freedom Technique (EFT) is another alternative treatment that has shown promising results in treating individuals struggling with PTSD and depression. EFT involves tapping various points on the body while reciting a mantra or phrase that acknowledges the individual’s current emotional state. The goal is to reframe one’s negative beliefs associated with trauma or depression to positive ones.
Studies have also shown that Eye Movement Desensitization and Reprocessing (EMDR) Therapy can help reduce symptoms of PTSD, especially when it happens alongside depression. This therapy involves safely recalling traumatic events while being subjected to specific external stimuli like moving lights or sounds.
Pro Tip: Remember that there isn’t one correct way of treating Co-occurring PTSD and Depression; different approaches may work for different individuals. It s best to experiment with various treatments to uncover what works best for you.
Your mental health matters – as does self-care! Next up – Self-Care Strategies for Co-occurring PTSD and Depression in Recovery, so buckle up and let s get more tips!
Self-Care Strategies for Co-occurring PTSD and Depression in Recovery
Every person in addiction recovery has a unique journey, with individual sets of challenges to overcome. For many, co-occurring PTSD and depression are particularly difficult hurdles to manage while navigating a path to sobriety. In this section, we’ll explore three self-care strategies that can help those who struggle with these co-occurring disorders while in recovery. We’ll take a closer look at the benefits of:
- Developing a healthy routine
- Practicing mindfulness
- Connecting with others
These strategies may not work for everyone, but they are a great starting point for managing co-occurring disorders in addiction recovery.

Developing a Healthy Routine for Managing Co-occurring PTSD and Depression
Developing a healthy routine for managing co-occurring PTSD and depression is crucial but can be challenging. However, it is achievable through implementing specific strategies to help address these conditions. Here are five points to consider.
- Firstly, it’s essential to establish a sleep schedule that works for you. Getting sufficient rest is crucial for your overall well-being, as lack of sleep can trigger symptoms of both PTSD and depression.
- Secondly, incorporating regular exercise into your routine can assist in alleviating the symptoms associated with PTSD and depression. Exercise promotes the release of endorphins which help boost mood and energy levels.
- Thirdly, practicing mindfulness techniques such as meditation, deep breathing exercises or yoga can aid in reducing stress and anxiety levels in those experiencing co-occurring PTSD and depression.
- Fourthly, establishing a healthy diet can also provide benefits for those managing these conditions. A balanced diet consisting of nutrient-dense foods such as fruits and vegetables can improve brain function while avoiding sugary foods and caffeine that aggravate symptoms.
- Lastly, scheduling time regularly to engage in leisure activities that bring joy or provide relaxation is essential for self-care when managing co-occurring PTSD and depression.
Developing a healthy routine for managing co-occurring PTSD and depression requires commitment; however, strategies such as getting enough sleep, regular exercise, mindfulness practice, healthy eating habits and leisure activities that bring joy are essential elements that contribute to maintaining emotional stability during recovery.
A true story reveals how poor management of co-occurring depression and PTSD led one recovering addict towards relapse. They focused exclusively on addiction recovery whilst neglecting their mental health issues. It taught them the importance of allowing themselves time to care for their mental health condition adequately.
Time spent learning breathing exercises became rewarding; they learned how to understand their emotions better by acknowledging sensations attached with each emotion they felt during mixing meditative techniques with journaling to evaluate their mood pockets. They developed practices around mindful exercise sessions at home and practiced meditation, where sudden traumatic things triggered regularly.
Mindfulness helps one contribute towards a healthier lifestyle, so I’m sharing six tips on practicing mindfulness in your daily life to aid recovery.
Practicing Mindfulness in Daily Life to Aid Recovery
Practicing Mindfulness in Daily Life to Aid Recovery is a powerful technique that can be used to address co-occurring PTSD and Depression in addiction recovery. It involves being present and fully engaged in the current moment, without judgment. By practicing mindfulness regularly, individuals can learn to identify and manage their emotions more effectively.
Mindfulness works by helping individuals develop a stronger sense of self-awareness. When we are mindful, we can recognize our thoughts and feelings as they arise, rather than getting lost in them or trying to avoid them altogether. This allows us to observe our emotions from a more objective perspective, which can help us break free from negative thought patterns.
Some valuable information about mindfulness includes its history and roots in Buddhist philosophy, as well as its growing popularity within Western psychology. It has been shown to be effective for reducing stress, anxiety, depression, and improving overall quality of life.
To practice mindfulness in daily life, try starting with simple practices such as focusing on your breath or paying attention to your physical movements while completing tasks. Other suggestions include practicing gratitude, setting intentions for your day or week ahead, and taking regular breaks throughout the day to check-in with yourself.
Incorporating mindfulness into your daily routine can take time but even small changes can make significant differences. Mindfulness helps one slow down racing thoughts and giving clarity around situations which we may have found overwhelming before. So next time when you sit down for a meal try not reaching out for your electronic devices instead get involved with your food, taste it feel its texture, cherish the moments of being alive!
Connecting with Others as a Vital Aspect of Coping with Co-occurring PTSD and Depression has its own unique set of challenges when it comes to recovery.
Connecting with Others as a Vital Aspect of Coping with Co-occurring PTSD and Depression
Connecting with others is important for coping with co-occurring PTSD and depression. Establishing social support helps individuals to deal with the issues related to trauma and depression in addiction recovery. People who suffer from co-occurring disorders often experience feelings of loneliness, alienation, and isolation. Therefore, connecting with others provides various benefits like validation, empathy, and a sense of belonging.
Connecting with others helps alleviate the symptoms of co-occurring PTSD and depression. Sharing experiences enables one to understand that they are not alone in their battle against these disorders. Many people can relate to each other’s experiences which bring about feelings of validation, acceptance and hope for recovery. Companionship creates a significant impact on emotions, mentality, physical wellness that facilitates coping strategies.
Social support is essential because it helps reduce negative impacts on mental health due to co-occurring PTSDs and depression. It offers a positive perspective while creating space for new resources or solutions during such harsh times in recovery from addiction management. Participation level in group therapies like CBT (Cognitive Behavioral Therapy), art therapy or joining support groups contributes immensely by providing a structure for establishing therapeutic connections.
A true story about this has been shared by many therapists who suggest group therapy as the successful approach for connecting with others in addiction recovery management programs an example among many is AA – Alcohol Anonymous or NA (Narcotic Anonymous) where experiencing companionship begets well-being which assures self-confidence then faithfulness results in continuous growth and progress.
Moving forward towards long-term management of co-occurring PTSD and depression needs some acute knowledge to start eliminating habits that lead to addiction gradually. The best way is to become your own therapist; self-care practices should be implemented each day as part of routine living decisions without dreading them.
Long-Term Management of Co-occurring PTSD and Depression
As someone who has personally struggled with co-occurring PTSD and depression during addiction recovery, I know how important it is to have a long-term management plan in place. One essential component of this plan is monitoring symptoms of both conditions, to ensure that they are being addressed in a proactive and holistic manner. Another crucial aspect is relying on a strong support system for continued recovery, as this can provide accountability, motivation, and encouragement during tough times. Lastly, seeking professional help as needed is critical to sustaining recovery from co-occurring PTSD and depression. In this section, we will explore each of these sub-sections in more detail, drawing on current research and best practices in addiction treatment.

Monitoring Symptoms of Co-occurring PTSD and Depression
When dealing with co-occurring PTSD and depression, monitoring symptoms is vital for effective long-term management. This involves checking for signs of both conditions in a systematic and ongoing manner, typically through regular assessments or check-ins with a medical professional or mental health provider.
Monitoring symptoms is crucial because PTSD and depression can often go hand-in-hand, meaning that the presence of one condition can exacerbate the other. It is also essential because these conditions can share many symptoms, making it challenging to distinguish between them without ongoing observation.
Some common symptoms of co-occurring PTSD and depression include difficulty sleeping, feelings of hopelessness or worthlessness, changes in appetite or weight, withdrawal from social activities, and recurrent negative thoughts or memories. By keeping an eye on these warning signs and others specific to each condition, healthcare providers can provide their patients with more targeted care.
It’s worth noting that monitoring symptoms is not a one-time event but an ongoing process throughout addiction recovery. Keeping track of any shifts in mood or behavior over time can help identify when intervention is necessary and ensure that patients receive the support they require.
If you’re currently in addiction recovery and dealing with co-occurring PTSD and depression, it’s crucial to monitor your symptoms regularly to ensure you receive the best possible care. Neglecting to do so could mean missing out on early interventions or overlooking significant changes that require attention.
As we’ve seen here, monitoring your symptoms is just one part of effectively managing co-occurring PTSD and depression. The next essential step involves relying on a strong support system for continued recovery – a topic we’ll discuss further in our next section.
Relying on a Strong Support System for Continued Recovery
Building a strong support system is critical for those in addiction recovery. With co-occurring PTSD and depression, this level of support can be even more helpful. Relying on a strong support system for continued recovery means surrounding oneself with individuals who care about their long-term health and sobriety.
Support systems work by providing a consistent source of encouragement and accountability. Those struggling with addiction often isolate themselves from loved ones, which can make it difficult to find the motivation to continue on the path to recovery. Support systems create a network of people who understand these struggles and are willing to offer both practical and emotional assistance.
One critical aspect of building a support system is finding individuals who understand the unique challenges that come with co-occurring PTSD and depression. These mental health conditions can exacerbate feelings of isolation and anxiety, making it essential to work with professionals who have experience treating similar cases.
When building a support system, it’s important not only to seek out family members or close friends but also those in 12-step programs or other rehabilitation groups. These groups offer an opportunity to connect with others on the same path, gaining valuable insight that can help individuals maintain their sobriety over time.
I once met a woman at a rehabilitation center who was recovering from alcohol addiction while also experiencing severe PTSD symptoms from past abuse. She shared how crucial her support network had been during her road to recovery, including her weekly counseling sessions, sponsor meetings, and group therapy sessions with fellow survivors of trauma. Through the connections she made in rehab, she found validation for her experience and learned valuable coping mechanisms for managing triggering situations.
Seeking Professional Help as Needed to Sustain Recovery from Co-occurring PTSD and Depression
Seeking professional help is a crucial step in sustaining recovery from co-occurring PTSD and Depression. It involves consulting with trained professionals such as therapists, psychiatrists, and addiction specialists to receive the appropriate treatment for both conditions. The process helps individuals deal with the challenges that come with battling both PTSD and Depression, which often arise during addiction recovery.
Professional help works through various methods, such as cognitive-behavioral therapy (CBT) and medication management. CBT helps individuals change their negative thought patterns and beliefs that contribute to their depression and anxiety. Medication management involves taking prescription drugs to alleviate symptoms, such as antidepressants or antianxiety medications. Alongside these treatments, support groups are also available to provide guidance and emotional support.
Seeking professional help has proven to be effective in sustaining recovery from co-occurring PTSD and Depression. It addresses the underlying causes of substance abuse while providing new avenues for coping with PTSD and Depression symptoms, reducing the likelihood of relapse. It also facilitates better communication between individuals in recovery and their loved ones. If you are looking for ways of addressing trauma in addiction treatment, professional help is definitely a step in the right direction.
Pro Tip: Seek around for affordable or free professional help options within your area. You can start by looking at government programs, local clinics providing healthcare services at minimal cost or other resources that can assist you when financial struggles hold you back. Remember, taking care of yourself should not come at an additional cost that hinders your wellbeing’s sustainability.
Five Facts About Addressing Co-occurring PTSD and Depression in Addiction Recovery:
- Co-occurring PTSD and depression are common among individuals seeking addiction recovery. (Source: National Institute on Drug Abuse)
- Integrated treatment for addiction and mental health disorders can lead to better outcomes and increased sobriety rates. (Source: Substance Abuse and Mental Health Services Administration)
- Trauma-focused therapies, such as cognitive processing therapy and prolonged exposure therapy, have been found to be effective in treating co-occurring PTSD and addiction. (Source: American Psychological Association)
- A holistic approach to treatment, addressing physical, mental, and emotional health, can be beneficial for individuals with co-occurring disorders. (Source: Journal of Substance Abuse Treatment)
- Ongoing support, such as therapy and support groups, can be important for maintaining sobriety and managing symptoms of PTSD and depression. (Source: Alcoholics Anonymous)
FAQs about How To Address Co-Occurring Ptsd And Depression In Addiction Recovery
1. How can I address co-occurring PTSD and depression in addiction recovery?
Addressing co-occurring PTSD and depression in addiction recovery may involve a comprehensive treatment plan that includes therapy, medication, support groups, and lifestyle changes. It is important to find a therapist who specializes in treating both PTSD and depression in addiction recovery. Additionally, medication management can help alleviate symptoms and support recovery.
2. What are some common symptoms of co-occurring PTSD and depression in addiction recovery?
Some Common symptoms of co-occurring PTSD and depression in addiction recovery are anxiety, irritability, low mood, panic attacks, nightmares, and intrusive thoughts. These can make it challenging to maintain abstinence from drugs or alcohol.
3. How does trauma impact addiction recovery?
Trauma can negatively impact addiction recovery by triggering cravings, increasing the risk of relapse, and making it difficult to cope with stressors and triggers.
4. Can medication be useful in addressing co-occurring PTSD and depression in addiction recovery?
Yes, medication can be helpful in reducing symptoms of PTSD and depression, allowing individuals to focus on their recovery. It is essential to work closely with a mental health professional to find the right medication regimen for each individual.
5. What kind of therapy is recommended for addressing co-occurring PTSD and depression in addiction recovery?
The kind of therapy that is recommended for addressing PTSD and depress in addiction is Cognitive-behavioral therapy (CBT), Eye Movement Desensitization and Reprocessing (EMDR), and dialectical behavior therapy (DBT) are all effective in treating co-occurring PTSD and depression in addiction recovery. It is important to find a therapist who specializes in trauma-focused therapies.
6. How can I support a loved one who is struggling with co-occurring PTSD, depression, and addiction?
You can support a loved one who is struggling with co-occurring PTSD, depression, and addiction by offering empathy, encouraging them to seek professional help, and providing practical support, such as transportation to appointments or help with daily tasks.