Have you ever wondered if the struggle with addiction is written in your DNA? How much does your genetic makeup dictate your potential for addiction? ‘Is addiction genetic?’ – this question sits at the intersection of nature and nurture. Delving into the science, research indicates that genetics accounts for roughly 40-60% of the risk for addiction. This article explores the intricate ways in which our genes may predispose us to addiction, without determining our destiny, and examines the critical role that environmental factors also play.
Key Takeaways
- Genetics account for 40-60% of an individual’s vulnerability to addiction, with dopamine levels and specific genes like ADH1B and CHRNA2 associated with substance use disorders; however, genetic predisposition is not deterministic.
- Environmental factors such as family dynamics, stressful life events, and co-occurring mental health issues significantly contribute to the risk of addiction, interacting with genetic susceptibility.
- Pharmacogenomics and personalized treatment strategies based on genetic profiles are emerging in addiction care, but raise ethical considerations regarding data privacy and require physicians to be trained in genetics.
The Role of Genetics in Addiction

Genetics plays a crucial role in understanding addiction. Studies suggest that 40-60% of an individual’s vulnerability to addiction can be attributed to genetic factors, with inherited dopamine levels playing a significant role. Dopamine, a key neurotransmitter in the brain, is associated with pleasure and reward, and its inherited levels can influence our susceptibility to addictive behaviors.
A family history of various issues including substance abuse, alcoholism, psychiatric illness, and criminal convictions can increase one’s genetic risk for drug abuse. However, possessing genes associated with addiction does not guarantee a person will develop a substance use disorder. It merely indicates a predisposition, not a certainty, much like having genes for heart disease doesn’t necessarily mean you’ll have a heart attack.
Key Addiction Genes
Certain genes can influence the risk of addiction to specific substances. For instance, the ADH1B and ALDH2 genes, involved in alcohol metabolism, can affect an individual’s risk of alcoholism. Variations in these genes can sometimes even provide a protective effect against alcohol use disorders. Other genes, such as GABRA2 and CHRM2, are strongly associated with alcohol use disorder, particularly linked to early onset alcoholism.
The influence of genetics is not limited to alcohol use. The CHRNA2 gene, for example, is implicated in cannabis use disorder, with lower expression levels associated with the condition. Furthermore, large-scale genetic studies have identified other influential genes such as CUL3, PDE4B, and PTGER3, which play a role in smoking and alcohol use behavior, suggesting a broader impact on substance use disorders.

Genetic Factors vs. Substance-Specific Factors
While some genetic factors influence addiction risk in a substance-specific manner, others contribute to general susceptibility. For example, the HIST1H2BD gene has been specifically associated with cocaine dependence, showing how specific genetic factors can be linked to addiction to certain substances. Similarly, alterations in genetic makeup, like the deletion of the mGluR2 receptor in rats, can lead to decreased sensitivity to the rewarding effects of cocaine, demonstrating gene-specific influences on drug response.
On the other hand, some genetic factors contribute to a more general susceptibility to addiction. One such example is the PSD-95 protein, encoded by the DLG4 gene, which has a regulatory role in dopamine-mediated synaptic and behavioral plasticity. This underscores a genetic contribution to general susceptibility to addictive behaviors, irrespective of the substance involved.
Alcohol Rehab South Carolina
Finding the right alcohol rehab in South Carolina can be a crucial step towards recovery for individuals struggling with alcohol addiction. South Carolina offers various rehabilitation centers equipped with tailored programs to address the specific needs of each individual. These facilities often provide a combination of medical treatment, therapy sessions, and support groups to help individuals overcome their addiction and develop coping mechanisms for long-term sobriety. Whether it’s inpatient or outpatient treatment, individuals can find options that suit their preferences and requirements. Additionally, many rehab centers in South Carolina offer aftercare programs to provide ongoing support and guidance to individuals as they transition back into their daily lives post-rehabilitation. It’s essential for those seeking help to research and choose a facility that aligns with their goals and needs for a successful recovery journey.
Environmental Factors and Addiction Risk

While genetics play a substantial role in addiction susceptibility, the environment also plays a crucial part. Stressful life changes, work-related stress, and the cumulative disadvantage of multiple stressors can prompt individuals to turn to substances as a coping mechanism, leading to substance abuse. The impact of these environmental factors can be amplified in those with a genetic predisposition to substance abuse, showcasing a significant interaction between one’s environment and genetics.
Factors that can significantly increase the risk of addiction include:
- Family dynamics, including the level of parental supervision, presence of family conflicts, divorce, or adverse childhood experiences
- Peer pressure
- Cultural norms and marketing strategies that normalize substance use
It is important to recognize that drug addiction risk is not solely a personal matter, but is also influenced by these external factors.
The Impact of Mental Health Issues
Mental health issues and substance use disorders often co-occur, presenting a complex challenge for treatment. Over a quarter of adults with serious mental health issues also have a substance use problem, indicating a high prevalence of co-occurring disorders. One of the reasons for this co-occurrence is self-medication, where individuals use substances to manage symptoms of mental health issues. For example, individuals with Post-Traumatic Stress Disorder (PTSD) may use substances as self-treatment for symptoms of trauma.
Stressful life events and poor coping skills can lead to increased impulsive responses, such as drug use and other forms of substance use for self-medication. Furthermore, shared genetic vulnerabilities, self-medication of symptoms, and related brain changes often contribute to the co-occurrence of mental health problems and substance use disorders. This relationship can also manifest through behavioral and social changes such as:
- frequent trouble
- secretive behaviors
- mood swings
- lack of motivation
- deterioration in appearance
- financial troubles
- changes in social circles
Early Life Experiences
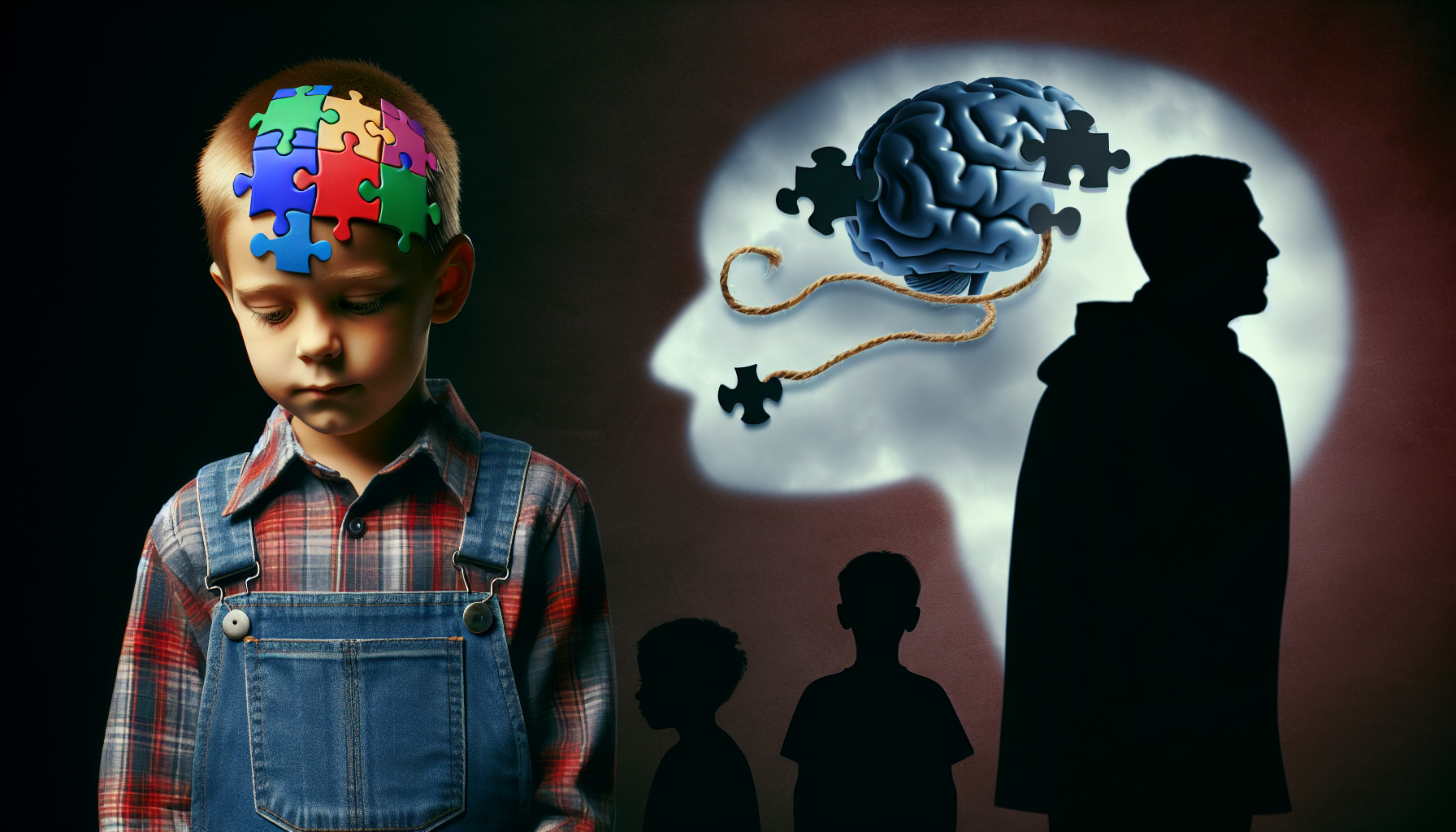
Early life experiences, including family environment and parental styles, can significantly impact addictive behaviors later in life. These experiences shape a person’s reaction to stress, understanding of normative behavior, and ability to regulate their emotions, all of which can contribute to their vulnerability to addiction. Younger individuals, whose brains are still developing, are especially vulnerable to substance use if their early social interactions involve substance use.
Cultural and religious teachings prevalent in early childhood can trigger addictive behaviors, sometimes in rebellion against certain cultural norms and upbringing. Moreover, young adults with a history of childhood adversity may exhibit decreased self-control and emotional regulation, which can lead to substance abuse as a result of their experiences and upbringing. It is crucial for these individuals to develop substance in their lives to overcome these challenges.
Is Addiction a Disease
The question of whether addiction is a disease has been a subject of debate within the medical and scientific communities. While addiction involves complex behavioral patterns and psychological factors, it is increasingly recognized as a chronic brain disorder characterized by compulsive substance use despite harmful consequences. Research indicates that addiction involves alterations in brain chemistry and function, affecting areas responsible for decision-making, impulse control, and reward processing. Furthermore, genetic predispositions and environmental factors can significantly influence an individual’s susceptibility to addiction. Viewing addiction through the lens of a disease can lead to more effective treatment approaches, emphasizing medical intervention, therapy, and support systems to manage symptoms and promote recovery. However, some critics argue that labeling addiction as a disease may absolve individuals of personal responsibility and overlook the role of choice and social determinants. Nonetheless, the consensus among many experts is that recognizing addiction as a disease helps reduce stigma and encourages a compassionate approach to addressing this pervasive public health issue.
Complex Interactions: How Genetics and Environment Influence Addiction

The interplay between genetics and environment is pivotal in understanding addiction. Genetic factors contribute to about half of a person’s risk of addiction, while the other half is influenced by environmental factors. High levels of chronic stress, for example, can alter genetic expression through a process called methylation, impacting the body’s stress response systems and potentially leading to a constant state of emergency in individuals.
This complex interplay between genetics and environment places particular demands on physicians, who need to evaluate the relative importance of multiple gene variants and their potential interactions with other drugs and environmental exposures. This is particularly crucial in understanding complex behaviors like addiction.
The Brain’s Reward System
Our brain’s reward system plays a crucial role in addiction, and genetic influences on this system can greatly impact addiction risk. Genetic influences on addiction risk partly overlap with other externalizing traits and disorders, hinting at a broader genetic vulnerability that impacts the brain’s reward system. High levels of dopamine, for instance, can exacerbate poor impulse control, thereby increasing the propensity for addictive behaviors.
Specific genes, like the MPDZ and CLOCK genes, have been associated with drug withdrawal responses and alcohol abuse, respectively. These multiple genes highlight the effects of specific genetic variations on the reward system. Moreover, single nucleotide variations and specific clock genes like those related to mGluR2 are linked to the increased risk of addiction and altered sensitivity to drug rewards, illustrating the genetic complexities affecting the reward pathways.
Stress Hormones and Addiction
Chronic stress can have profound effects on the brain and behavior, contributing to the development of addiction. Some of the effects of chronic stress include:
- Reduction in gray matter volume in brain areas that control cognitive processing and stress response
- Impaired impulse control
- Increased incidence of using substances as a coping mechanism
Chronic stress is a key contributor across the stages of addiction, impacting the onset, persistence, and risk of relapse. It also poses challenges in achieving positive treatment results.
Early life trauma can also critically affect the vulnerability to addiction later in life through alterations in the genetic regulation of the body’s stress response systems. Such alterations can lead to impaired stress management capabilities, thereby increasing the susceptibility to addiction.
Genetic Testing and Personalized Treatment
While understanding the genetic and environmental factors influencing addiction is crucial, applying this understanding to improve treatment strategies is equally important. Pharmacogenomics, the study of how genes affect a person’s response to drugs, aims to enable physicians to match individual patients to the substance abuse treatment that will work best for them, considering both their genetic profile and other factors. Genetic testing can identify the safest and most effective addiction treatments for individual patients, potentially leading to significant improvements in treatment outcomes by tailoring medication to an individual’s specific genetic makeup.
However, a substantial challenge to the implementation of pharmacogenomic treatments in addiction care is the readiness of primary care physicians, who often lack formal training in genetics and are typically the first to treat addiction. Therefore, it is crucial to equip physicians with the necessary skills and knowledge to effectively use genetic information in addiction treatment.
Understanding Genetic Information
To tailor addiction treatments effectively, physicians require clear and accessible guidelines that leverage genetic information. These guidelines need to be supported by decision tools integrated with electronic health record systems. This will enable physicians to make informed decisions about treatment strategies based on a comprehensive understanding of the patient’s genetic information and overall condition.
Ethical Considerations in Genetic Testing
While genetic testing holds promise for improving addiction treatment, it also raises several ethical considerations. The sensitive nature of genetic information necessitates strict data privacy and confidentiality measures to protect patient information. Genetic information not only pertains to the individual being tested but also provides information about their relatives, raising significant privacy concerns.
Furthermore, ensuring the responsible storage of genetic information in biobanks and medical records poses challenges for informed consent procedures. The revelation of genetic predispositions in addiction treatment can increase the risk of stigmatization and expose individuals to discrimination by health insurers or employers.
Thus, the ethical landscape of pharmacogenomics in addiction treatment encompasses various considerations including safeguarding privacy, mitigating potential discrimination, and involving patients in treatment decisions.
What Are Schedule 4 Drugs
“What are schedule 4 drugs” refers to a classification within the Controlled Substances Act (CSA) of the United States. Schedule 4 drugs are substances that have a recognized medical use but also have a potential for abuse or dependence, although less so than drugs in higher schedules. Examples of schedule 4 drugs include certain prescription medications such as Xanax (alprazolam), Valium (diazepam), and Ambien (zolpidem). These drugs are typically prescribed for conditions like anxiety, insomnia, or panic disorders. Despite their medical benefits, they are regulated due to their potential for misuse or addiction. Physicians must carefully monitor their use to mitigate risks and ensure patient safety.
Overcoming Addiction: Treatment Options and Support

Overcoming addiction requires a comprehensive approach that addresses both the genetic and environmental factors contributing to the disorder. Effective treatment for substance use disorders, particularly when co-occurring with mental health issues, requires an individualized approach that may include:
- Rehabilitation
- Medication
- Talk therapy
- Support groups
Peer support groups, when used alongside professional treatments, provide a well-rounded strategy for achieving and maintaining sobriety.
Inpatient vs. Outpatient Treatment
When considering treatment options, the choice between inpatient and outpatient treatment depends largely on the individual’s needs. Inpatient treatment involves staying in a residential facility full-time, providing continuous support and structured accountability. This intensive form of treatment can be particularly beneficial for individuals with severe substance use disorders or those with co-occurring mental health conditions.
On the other hand, outpatient treatment allows patients to maintain their regular schedule, including work and home responsibilities, while receiving treatment during prescribed times. This flexibility can make outpatient treatment an attractive option for individuals who need to balance treatment with other responsibilities. However, the cost of treatment, whether inpatient or outpatient, can vary significantly depending on the services needed and insurance coverage.
Finding the Right Support
Finding the right support is a crucial component of the recovery process. Peer support groups such as Narcotics Anonymous (NA), endorsed by the National Institute, provide important emotional support for individuals recovering from addiction, facilitating connections with others in similar situations. NA employs a 12-step program and encourages member sponsorship, which is associated with maintaining long-term abstinence.
There are also substance-specific support groups like Cocaine Anonymous and Marijuana Anonymous that utilize a 12-step approach akin to Narcotics Anonymous. Other groups like Secular Organizations for Sobriety (SOS) focus on providing a nonreligious environment that emphasizes self-empowerment in achieving and maintaining sobriety. Similarly, SMART Recovery offers a program centered around self-management, while LifeRing Secular Recovery promotes personally tailored recovery approaches.
Summary
In conclusion, addiction is a complex disease influenced by an intricate interplay of genetic and environmental factors. Understanding these influences can help tailor more effective and personalized treatment strategies. However, the successful implementation of these strategies requires overcoming several challenges, including equipping healthcare providers with the necessary skills, addressing ethical concerns related to genetic testing, and ensuring the availability of comprehensive support systems.
Frequently Asked Questions
Is addiction a genetic thing?
While genetics play a significant role in a person’s risk of addiction, it is also influenced by environmental factors. Research suggests that more than half of the differences in likelihood of developing substance use problems stem from DNA differences (Smith, 2022).
Is there a gene for alcoholism?
Yes, genes related to alcohol metabolism, such as ADH1B and ALDH2, are closely tied to the risk of problem drinking, and a family history of alcohol use disorders can increase the risk of a genetic predisposition to developing an alcohol use disorder.
What causes an addictive personality?
An addictive personality is often linked to genetics, with research showing that individuals born to addicted parents are more likely to exhibit addictive behavior and tendencies. This can be a significant factor in understanding the causes of addictive personalities.
How do environmental factors influence addiction risk?
Environmental factors such as stress, family dynamics, and peer pressure can significantly increase the risk of addiction, especially in individuals with a genetic predisposition to substance abuse.
What are some considerations in choosing between inpatient and outpatient treatment?
The choice between inpatient and outpatient treatment depends on the individual’s needs and responsibilities. Inpatient treatment provides continuous support and structured accountability, while outpatient treatment allows patients to maintain their regular schedule while receiving treatment during prescribed times.