Federal guidelines for opioid treatment programs are essential regulatory standards that ensure the provision of appropriate care to individuals struggling with opioid addiction. These guidelines aim to establish a comprehensive framework for the treatment and management of opioid use disorder, prioritizing patient well-being and safety.
This article will delve into the Federal Guidelines for Opioid Treatment Programs, outlining the regulatory standards that govern their operations. It will cover aspects such as accreditation and certification requirements, staffing and qualifications, patient assessment and treatment planning, medication dispensing, and administration, coordination of care, and quality improvement and performance measurement.
Compliance with these guidelines is of utmost importance to ensure effective and standardized care for individuals seeking treatment for opioid addiction. However, implementing these guidelines may pose several challenges, including financial constraints, workforce shortages, and stigma and misconceptions surrounding opioid addiction.
By exploring these topics, this article aims to shed light on the significance of federal guidelines for opioid treatment programs and the hurdles faced in their implementation.

What are Opioid Treatment Programs?
In the United States, the rates of drug overdose deaths are consistently rising, with opioids being the primary driver of this crisis which has been discussed in Disparities in Access to Opioid Treatment Programs and Office-Based Buprenorphine Treatment Across the Rural-Urban and Area Deprivation Continua by Amiri et al.,. Opioid Treatment Programs (OTPs) are healthcare centers that provide treatment for opioid addiction. These programs help individuals overcome dependence on opioids and achieve long-term recovery. In OTPs, patients receive evidence-based treatments, including medication-assisted therapy (MAT), counseling, and support services. MAT involves using medications like methadone, buprenorphine, or naltrexone to reduce opioid cravings and withdrawal symptoms, allowing patients to focus on recovery and rebuild their lives without the constant struggle of addiction.
OTPs follow strict regulatory standards to ensure safe and effective treatment. These standards cover medication administration, counseling requirements, and patient monitoring. Compliance with these standards is crucial for the quality of care and patient well-being.
John, a 35-year-old struggling with opioid addiction, found hope and healing in an OTP. After years of substance abuse, he entered the program to break free from addiction. Through comprehensive care and support, John received the medication and counseling needed to address his addiction’s physical and psychological aspects. The program empowered him to rebuild his life, repair relationships, and regain self-confidence. Today, John lives a fulfilling life free from opioids, thanks to the treatment and support from the OTP.
What is the Purpose of OTPs?
The purpose of OTPs, or Opioid Treatment Programs, is to provide care and treatment for individuals with opioid addiction. OTPs help patients recover and improve their well-being. Here are the key aspects of OTPs:
1. Support Recovery: OTPs help individuals recover from opioid addiction. They provide a safe environment for evidence-based treatments and interventions.
2. Reduce Harmful Effects: OTPs aim to minimize the harmful effects of opioid addiction. By offering medication-assisted treatment, such as methadone or buprenorphine, OTPs help minimize withdrawal symptoms and cravings, enabling patients to lead productive lives. As explained by Winstanley, PhD et al., in Improving treatment for opioid dependence, there are two types of medications for opioid dependence: detoxification medications, which are used short-term to alleviate withdrawal symptoms, and maintenance medications, which are used long-term to prevent relapse into drug use.
3. Improve Functioning and Quality of Life: OTPs focus on enhancing patients’ functioning and quality of life. Through counseling, therapy, and support services, OTPs help individuals address underlying factors contributing to their addiction and develop strategies for relapse prevention.
4. Enhance Community Safety: OTPs contribute to the overall safety and well-being of the community. By reducing opioid misuse and related criminal activities, OTPs promote public health and safety.
5. Promote Holistic Care: OTPs prioritize holistic care, addressing physical, psychological, and social aspects of opioid addiction. They tailor treatment to individual needs.
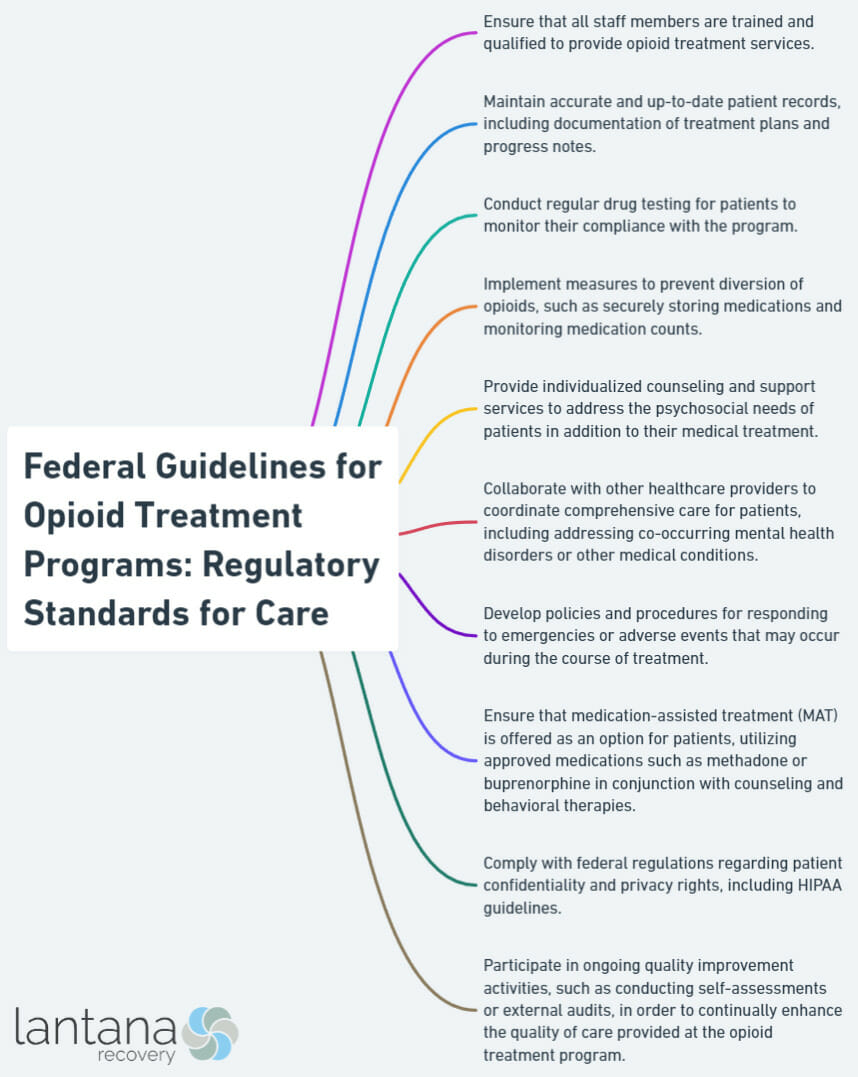
Regulatory Standards for Opioid Treatment Programs
When it comes to ensuring effective and safe treatment for those battling opioid addiction, regulatory standards play a pivotal role. In this section, we’ll dive into the critical components of regulatory standards for opioid treatment programs. From the requirements for accreditation and certification to staffing and qualifications, patient assessment and treatment planning, dispensing and administration of medications, coordination of care, and quality improvement and performance measurement, we’ll explore the key aspects that contribute to the delivery of high-quality care in these programs. Get ready to discover the standard-setting journey!
Requirement for Accreditation and Certification
Accreditation and certification are requirements for an Opioid Treatment Program (OTP) to operate. These ensure that the program meets federal guidelines and necessary standards.
Accreditation evaluates and verifies that an OTP meets specific quality standards, recognizing excellence and ensuring safe and effective patient care. Certification, on the other hand, is the governing body’s official recognition that the OTP meets all necessary requirements. Both accreditation and certification are crucial requirements for the success and legitimacy of an OTP.
Accreditation and certification guarantee that the program meets criteria in staffing, qualifications, patient assessment, treatment planning, medication administration, care coordination, and quality improvement. Adhering to these requirements ensures the highest level of care for individuals with opioid addiction.
Obtaining accreditation and certification involves assessments, audits, and inspections. It demonstrates the program’s commitment to quality care and continuous improvement, ensuring patient safety and community confidence.
OTPs must understand and comply with the requirement for accreditation and certification to contribute to the effectiveness and success of opioid treatment programs, helping individuals overcome addiction and improve their quality of life.
Historically, accreditation and certification in healthcare settings ensure high-quality care and patient safety. These programs emerged in the early 1900s to standardize practices and hold providers accountable. Today, accreditation and certification serve as essential benchmarks for evaluating the quality and performance of healthcare organizations, including OTPs.
Staffing and Qualifications
Staffing and qualifications play a critical role in opioid treatment programs (OTPs) when it comes to delivering safe and effective care to patients. In order to achieve this, OTPs must have a sufficient number of highly qualified healthcare professionals. This includes medical doctors, nurses, counselors, and addiction treatment specialists. These staff members should possess expertise and training in opioid addiction treatment, as well as a thorough understanding of evidence-based practices and medications such as methadone and buprenorphine.
To ensure that staff members remain up-to-date with the latest advancements and best practices in opioid addiction treatment, OTPs should provide ongoing training and professional development opportunities. It is essential for staff to stay informed and knowledgeable in order to provide the best possible care.
In addition, staff should receive appropriate supervision and have ample opportunities for collaboration with their colleagues. This fosters a multidisciplinary approach to patient care, which is an invaluable aspect of the treatment process.
By prioritizing adequate staffing and qualifications, OTPs can offer comprehensive and high-quality care to individuals who are struggling with opioid addiction. This includes conducting proper evaluations, developing individualized treatment plans, administering medication, coordinating care, and continuously striving for quality improvement.
Patient Assessment and Treatment Planning
Patient assessment and treatment planning are essential components of opioid treatment programs (OTPs). Healthcare professionals like Lantana Recovery play an active role in evaluating and designing treatment plans to ensure the best possible outcomes and well-being for patients.
Throughout the assessment process, healthcare providers gather information about the patient’s medical history, substance use patterns, and mental health conditions. This information helps identify their specific needs and challenges, which then serves as the basis for a customized treatment plan.
Treatment planning involves developing an individualized plan based on the findings from the assessment. This plan includes determining the most suitable medication-assisted treatment (MAT), dosage, duration, and additional supportive services such as counseling, therapy, and social support. The plan is regularly reviewed and adjusted to ensure optimal progress.
Opportunities to enhance patient assessment and treatment planning in OTPs include utilizing standardized tools and guidelines, promoting interprofessional collaboration, and taking patient preferences into account. By incorporating these elements, OTPs can provide comprehensive and patient-centered care.
It’s important to emphasize that patient assessment and treatment planning are ongoing processes that require continuous evaluation and adjustments to meet evolving needs. Through individualized care and evidence-based practices, OTPs can effectively support patients in their journey toward recovery.
Dispensing and Administration of Medications
When dispensing and administering medications in opioid treatment programs, healthcare providers must take into account the following important factors:
1. Accuracy: Providers must strictly adhere to precise dosing protocols and guidelines in order to ensure the safe and effective administration of medications.
2. Record-keeping: It is crucial to maintain accurate documentation for tracking the medications that are dispensed, the doses that are administered, and any potential side effects or reactions that may occur.
3. Patient education: Providers should educate patients on the proper techniques for administering medications, as well as inform them about potential side effects and emphasize the importance of following their treatment regimens.
4. Monitoring and follow-up: Ongoing monitoring and regular follow-up appointments are necessary in order to assess the progress of patients, identify any issues that may arise, and make adjustments to their treatment plans if necessary.
By effectively dispensing and administering medications in opioid treatment programs, healthcare providers can greatly contribute to achieving successful outcomes, promoting overall well-being, and facilitating the recovery of patients from addiction.
It is a well-established fact that adherence to medication protocols in opioid treatment programs significantly reduces the risk of relapse and improves long-term recovery rates. A study published in the Journal of Addiction Medicine revealed that such adherence can lead to an impressive improvement of up to 60% in recovery rates.
Coordination of Care
Coordination of care is crucial in opioid treatment programs (OTPs). Effective coordination ensures that patients receive comprehensive care that meets their needs and supports their recovery. Here are key considerations for the coordination of care in OTPs:
1. Collaborative approach: Coordinating care requires collaboration among healthcare providers, counselors, and other professionals like Lantana Recovery involved in treating individuals with opioid use disorder. This multidisciplinary approach ensures well-coordinated and cohesive care.
2. Communication: Clear and effective communication is essential for coordination of care. This involves sharing information and updates among the treatment team, including progress, medication adjustments, and challenges. Regular communication helps identify gaps in care and allows for timely interventions.
3. Referrals and continuity: Coordinating care includes facilitating appropriate referrals to additional services or specialists as needed. This may involve connecting patients with mental health support, vocational training, residential support like substance abuse inpatient treatment, or social services to improve their overall well-being.
4. Patient-centered approach: Coordinating care should prioritize the preferences and goals of the patient. It involves actively engaging patients in their treatment plans, providing comprehensive information, and involving them in decision-making processes to align treatment with their values and preferences.
5. Monitoring and follow-up: Regular monitoring and follow-up are essential components of care coordination. This includes monitoring medication adherence, addressing side effects or concerns, and conducting regular check-ins to assess the progress of individuals in treatment.
Quality Improvement and Performance Measurement
Quality improvement and performance measurement play a crucial role in ensuring the effectiveness and success of opioid treatment programs (OTPs). These programs aim to offer comprehensive care to individuals with opioid addiction.
In order to enhance the quality of care in OTPs, they implement continuous quality improvement initiatives. This entails monitoring performance indicators and gathering data to assess the effectiveness of the program. Key metrics, such as treatment retention rates, successful outcomes, and patient satisfaction, are regularly evaluated to identify areas that need improvement.
The performance indicators, data collection methods, and measurement frequency for OTPs are as follows:
- Treatment retention rates: Electronic health records (monthly).
- Successful outcomes: Follow-up surveys (quarterly).
- Patient satisfaction: Anonymous feedback forms (annually).
By measuring performance, OTPs can compare their results to national benchmarks and standards. This helps them understand their position and identify areas for improvement or excellence. Additionally, it enables evidence-based decision-making and the implementation of proven strategies and interventions.
By prioritizing quality improvement and performance measurement, OTPs can continuously improve their services to offer the highest level of care and support to individuals seeking treatment.
For instance, one OTP noticed a significant dropout rate in their program. They identified challenges in medication adherence as the primary reason. To address this issue, they implemented interventions such as medication reminders, counseling sessions, and ongoing support. As a result, the dropout rate decreased by 30% within six months, leading to improved treatment outcomes and increased patient satisfaction.

Importance of Compliance with Federal Guidelines
“Opioid treatment programs (OTPs) serve as daily essential services for people with opioid use disorder” (Opioid treatment program safety measures during the COVID-19 pandemic: a statewide survey, Bandara et al., 2022) and play a crucial role in addressing the opioid crisis and providing evidence-based treatment options.
Compliance with federal guidelines is crucial in opioid treatment programs. It ensures safe and effective care for individuals seeking treatment. The importance of compliance with federal guidelines can be understood through several key points:
-
Patient safety: Compliance with federal guidelines guarantees the safety of patients undergoing opioid treatment. Following these standards minimizes the risks associated with opioid medications and ensures appropriate care.
-
Quality of care: Adhering to federal guidelines enhances the overall quality of care provided in opioid treatment programs. Following these standards ensures evidence-based treatments, leading to improved outcomes and higher patient satisfaction.
-
Regulatory requirements: Compliance with federal guidelines is essential to meet governing bodies’ regulatory requirements. Opioid treatment programs must adhere to these guidelines to maintain their legal standing and avoid penalties or sanctions.
-
Standardization: Federal guidelines help standardize the care provided across different opioid treatment programs. This consistency ensures that patients receive consistent treatment regardless of the location or facility they seek help.
-
Accountability: Compliance with federal guidelines holds opioid treatment programs accountable for their actions and practices. It ensures transparency and ethical behavior, protecting the welfare of patients and promoting public trust.
-
Continuity of care: Following federal guidelines allows opioid treatment programs to ensure a smooth transition of care for patients. Consistency in protocols and practices allows for seamless collaboration between healthcare providers involved in a patient’s treatment journey.
Compliance with federal guidelines is vital in opioid treatment programs as it promotes patient safety, maintains the quality of care, meets regulatory requirements, standardizes practices, ensures accountability, and facilitates continuity of care.

Challenges in Implementing Federal Guidelines
Implementing federal guidelines for opioid treatment programs comes with its fair share of challenges. From financial constraints to workforce shortages and the persistence of stigma and misconceptions, navigating these obstacles can be an uphill battle. In this section, we’ll delve into the difficulties healthcare providers face when trying to adhere to these regulatory standards, shedding light on the complexities that hinder effective implementation. Get ready to explore the real-world hurdles that impact the delivery of quality care to those in need.
Financial Constraints
Financial constraints can pose significant challenges to implementing federal guidelines in opioid treatment programs. These constraints can impact various aspects, including access to medications, staffing and training, facilities and equipment, support services, and coordination of care.
Insufficient funding can result in delays or limitations in providing essential medications to patients. Additionally, it can hinder the recruitment and retention of qualified staff members, leading to workforce shortages and a lack of opportunities for training. Moreover, financial constraints may restrict the improvement or expansion of treatment facilities, resulting in overcrowding, inadequate resources, and outdated equipment.
The availability and quality of crucial support services, such as counseling and social support, can also be hindered due to limited funding. Furthermore, coordinating care among healthcare providers becomes increasingly challenging when financial resources are limited, ultimately leading to fragmented or incomplete care for patients.
To ensure the successful implementation of federal guidelines in opioid treatment programs, it is imperative to address these financial constraints. By increasing funding and allocating more resources, we can overcome these challenges and provide better care for individuals grappling with opioid addiction.
Workforce Shortages
Workforce shortages in opioid treatment programs can present challenges to providing adequate care and support to individuals facing opioid addiction. These shortages can affect the efficiency and effectiveness of treatment programs, leading to long wait times, limited access to care, and increased strain on staff.
One issue contributing to workforce shortages is the insufficient number of healthcare professionals trained in addiction medicine and specialized techniques for opioid treatment. The shortage of doctors, nurses, and counselors with expertise in this field can hinder comprehensive care.
With limited staff, each healthcare professional often has to handle a larger workload, leading to burnout and decreased job satisfaction. This can compromise the quality of care and contribute to attrition rates within treatment programs.
Workforce shortages in opioid treatment programs are more apparent in rural and underserved areas. Limited access to healthcare professionals can result in disparities in treatment availability and hinder efforts to combat the opioid crisis.
When there are not enough healthcare professionals available, individuals seeking help may experience delays in accessing care, leading to exacerbated health issues and an increased risk of relapse.
Addressing workforce shortages in opioid treatment programs requires a multi-faceted approach. This includes increasing training and education opportunities for healthcare professionals in addiction medicine, offering incentives to attract and retain qualified staff, and improving resources and infrastructure in underserved areas.
In recent years, the opioid crisis has reached alarming levels, with a significant increase in opioid-related deaths and addiction rates. As the demand for opioid treatment programs has surged, so has the need for a well-trained and sufficient healthcare workforce to provide care and support. Efforts are being made to address these workforce shortages, including increased funding for training and education programs, expanding access to certification programs, and implementing policies to attract professionals to this specialized area of healthcare. It is crucial to continue investing in strategies that cultivate a skilled and resilient workforce to ensure comprehensive and accessible care for individuals struggling with opioid addiction. The dedication and commitment of healthcare professionals working in opioid treatment programs are vital in combatting this crisis and saving lives.
Stigma and Misconceptions
Stigma and misconceptions hinder effective care and support for individuals with opioid addiction whether inpatient or outpatient treatment programs are chosen for substance abuse recovery. These beliefs can prevent people from seeking treatment, discourage healthcare professionals from providing support, and perpetuate harmful stereotypes about addiction.
One common misconception is that people in opioid treatment programs are weak or morally flawed. This overlooks the fact that addiction is a complex disease that can affect anyone. Seeking help and participating in treatment programs requires courage and should be applauded.
Another misconception is that medication-assisted treatment, a commonly used approach in opioid treatment programs, simply replaces one addiction with another. This fails to acknowledge the evidence-based nature of these treatments, which have been extensively studied and proven effective in reducing cravings, preventing overdoses, and promoting long-term recovery.
To address these misconceptions, education, and awareness campaigns are crucial. Providing accurate information about opioid addiction, treatment options, and success rates can dispel stigmas and foster a more compassionate and supportive society.
Combating stigma and misconceptions requires promoting a comprehensive understanding of addiction as a medical condition that requires evidence-based treatment and support. By challenging negative beliefs and encouraging open dialogue, we can create an environment that fosters empathy, understanding, and ultimately, the recovery and well-being of individuals affected by opioid addiction.
True Story: Sarah, a young woman struggling with opioid addiction, faced significant stigma and misconceptions when she entered an opioid treatment program. Friends and family questioned her commitment and accused her of taking the “easy way out.” However, with the support of healthcare professionals like Lantana and peer groups, Sarah overcame these barriers and successfully completed her treatment program. Today, she leads a fulfilling life free from opioid addiction and is passionate about raising awareness and fighting the stigma associated with addiction.
As stated by researchers Erin L. Winstanley et al., in a 2015 study titled Improving treatment for opioid dependence, opioid dependence medications can serve two main purposes: short-term use to alleviate withdrawal symptoms (detox meds) and long-term use to prevent relapse into drug use (maintenance meds). Success stories highlight the importance of addressing stigma and misconceptions to ensure that individuals receive the care and support they need to overcome addiction.
Frequently Asked Questions
What are the requirements to access FederalRegister.gov & eCFR.gov?
To access FederalRegister.gov & eCFR.gov, you need to request access by adding your IP address to a set of IPs that can access these sites. As a human user, you will need to complete a CAPTCHA (bot test) and click “Request Access”. This process needs to be repeated for each IP address you want to access the site from, and the requests are valid for approximately three months.
How can I request access for a wider IP range to FederalRegister.gov & eCFR.gov?
If you want to request access for a wider IP range, you should first request access for your current IP and then use the “Site Feedback” button to make the request. By following this process, you can request access to a wider IP range of these sites.
What are the Federal Guidelines for Opioid Treatment Programs?
The Federal Guidelines for Opioid Treatment Programs provide guidance on various aspects of opioid treatment, including patient assessment, treatment planning, medication-assisted treatment, overdose and relapse prevention, and recovery care. These guidelines aim to ensure high-quality care for individuals with opioid use disorder.
Do I need certification to dispense medications for the treatment of substance use disorders?
Yes, certification is required to dispense medications for the treatment of substance use disorders. Any deviation from the federal standards requires the submission and approval of an exception request.
Are there any training materials and resources available for medical professionals in opioid treatment?
Yes, there are training materials and resources available for medical professionals in opioid treatment. These resources include an OTP certification application, a pocket guide on medication-assisted treatment of opioid use disorder, a mobile app for practitioners providing medication-assisted treatment, and all SAMHSA publications on medication-assisted treatment.
How does the DEA present best practices for narcotic treatment programs?
The DEA presents best practices for narcotic treatment programs, which cover various aspects such as ordering and dispensing medication, recordkeeping, and security measures. These practices aim to ensure the safe and effective delivery of medication-assisted treatment for opioid use disorder.









