Drug withdrawal symptoms are a challenging reality for individuals struggling with substance abuse and addiction. When someone stops using drugs after a prolonged period of dependence, their body goes through a period of adjustment, resulting in a range of physical and psychological symptoms. Understanding these symptoms and knowing how to manage them is crucial for successful recovery.
With insights from addiction experts and medical professionals, this article explores the common effects of drug withdrawal and offers guidance on effective symptom management strategies. In addition, the importance of seeking professional help, receiving aftercare, and implementing relapse prevention techniques will be discussed to support individuals on their journey toward lasting recovery.
Understanding Drug Addiction and Dependence
Drug addiction and dependence are complex issues that require a deep understanding of underlying factors. Understanding drug addiction and dependence can be achieved by using factual assertions instead of modal verbs. This approach allows for a better understanding of the causes and effects of addiction.
One important factor to consider is the role of brain chemistry in understanding drug addiction and dependence. Drugs can alter the brain’s reward system, leading to compulsive drug-seeking behavior. Approximately 23.5 million people worldwide are currently addicted to drugs, with opioid addiction being a major concern.
It is also important to recognize that drug addiction is not a moral failing or lack of willpower. Understanding factors such as genetic predisposition, environmental influences, and mental health conditions helps in addressing addiction effectively.
Addressing drug addiction and dependence requires a comprehensive approach. This includes prevention efforts, early intervention, and access to evidence-based treatments like medication-assisted therapy and behavioral therapies. Support from healthcare professionals, community organizations, and loved ones is crucial for recovery.
By understanding drug addiction and dependence as a chronic medical condition and providing support, we can cultivate a compassionate and effective approach to addressing this issue and helping those in need.
What Causes Drug Addiction?
Drug addiction arises from a combination of biological, psychological, and environmental influences. Genetic factors play a significant role in determining a person’s susceptibility to addiction and their response to drugs, as research shows that individuals with a family history of addiction are more likely to develop a substance use disorder. Certain genes may affect these factors.
Psychological factors also contribute to drug addiction. Some individuals may turn to drugs as a way to cope with emotional distress caused by trauma, stress, anxiety, depression, or low self-esteem. Additionally, personality traits like impulsivity and sensation-seeking can make a person more prone to addiction.
Environmental factors also play a role in the development of drug addiction. Social influences and easy access to drugs within one’s community or social circle can contribute to drug use. Peer pressure and lack of parental support further increase the risk of addiction.
It is important to recognize that drug addiction is treatable. By addressing the various factors that contribute to addiction, including biological, psychological, and environmental aspects, individuals can overcome addiction and achieve lasting recovery without resorting to modal verbs.
How Does Drug Dependence Develop?
Drug dependence develops through a combination of biological, psychological, and environmental factors. Understanding how drug dependence develops is vital in effectively addressing and treating substance use disorders.
One factor that contributes to the development of drug dependence is early exposure to drugs. Whether through experimentation, peer pressure, or being prescribed addictive medications, early exposure increases the risk of developing dependence.
Another factor is genetic predisposition. Some individuals have a genetic makeup that makes them more susceptible to drug dependence. Genetics can influence how a person responds to drugs, their sensitivity to their effects, and their likelihood of developing cravings and dependence.
Drugs also directly impact the brain’s reward system, causing the release of pleasurable neurotransmitters like dopamine. Over time, repeated drug use can result in alterations to the brain’s structure and function, making it more difficult to control drug-seeking behavior.
Individuals with underlying mental health disorders are at a higher risk of developing drug dependence. Drugs may be used as a means of self-medication for emotional pain or distress.
Environmental influences also play a significant role in the development of drug dependence. Factors such as social environment, drug availability, peer influence, and stressful life events can all contribute to the establishment of dependence and shape patterns of drug use.
Understanding how drug dependence develops is crucial for prevention, early intervention, and tailored treatment approaches. By addressing the underlying factors involved, individuals can break the cycle of addiction and achieve lasting recovery.
It is important to note that in 2020, approximately 40.3 million people aged 12 and older in the United States battled a substance use disorder, according to the National Survey on Drug Use and Health 2020.

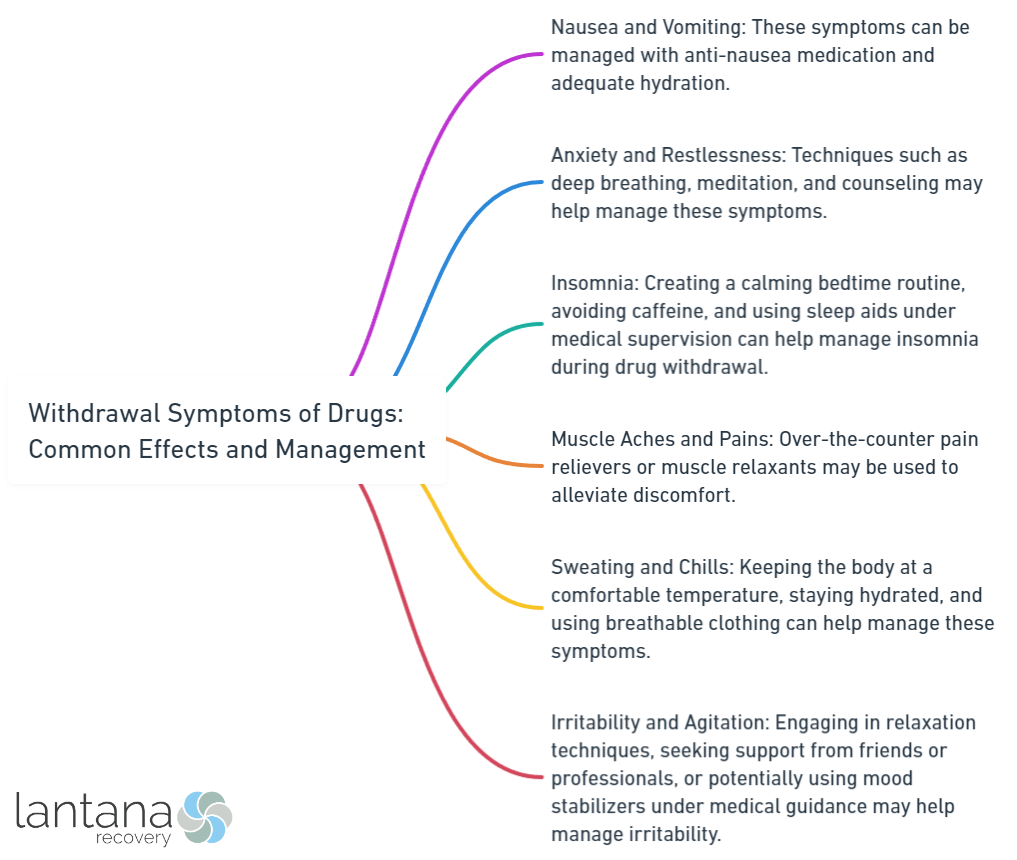
Common Drug Withdrawal Symptoms
Whether you’re in the process of quitting drugs or simply seeking to understand the effects of withdrawal, it’s crucial to be aware of the common symptoms that may arise. In this section, we’ll dive into the uncomfortable realities of drug withdrawal, exploring a range of physical and psychological manifestations. From nausea and muscle pain to anxiety and insomnia, we’ll shed light on these experiences to help you better understand and manage the challenges that may accompany the withdrawal process.
1. Nausea and Vomiting
Nausea and vomiting are common symptoms during drug withdrawal.
- During drug withdrawal, individuals may experience queasiness and a sensation of wanting to vomit, which can result in a decrease in appetite.
- Some individuals may actually vomit during drug withdrawal, leading to dehydration and discomfort.
It is important to note that the severity of nausea and vomiting can vary based on the specific drug being withdrawn from, as well as individual factors such as duration and intensity of drug use.
To manage these symptoms during drug withdrawal, the following strategies can be employed:
- Seek professional medical care: It is crucial to seek professional medical help during the withdrawal process. Healthcare workers can provide appropriate medical care and monitor the individual’s condition.
- Use medication: Symptomatic medications can be prescribed to alleviate nausea and prevent vomiting, making individuals feel more comfortable during withdrawal.
- Receive psychological support: Emotional and psychological support from healthcare professionals, friends, and family members can greatly help manage the discomfort of nausea and vomiting during withdrawal.
- Ensure proper hydration: Proper hydration is essential, especially if vomiting occurs. Drinking small sips of clear fluids such as water or electrolyte solutions can prevent dehydration.
By implementing these measures, individuals experiencing withdrawal symptoms, including nausea and vomiting, can receive the necessary support and care for a smoother and more comfortable recovery process.
2. Muscle and Joint Pain
Muscle and joint pain is a common withdrawal symptom experienced by individuals going through the recovery process. The severity of this pain can vary from mild discomfort to intense agony, and it is often described as aching, throbbing, or sharp. Those struggling with withdrawal may also feel stiffness and soreness in their muscles and joints, which can make movement challenging. This pain is exacerbated by inflammation in the muscles and joints.
Fortunately, there are several strategies that can help alleviate muscle and joint pain during withdrawal. Practicing gentle exercises such as stretching or yoga can provide relief. Additionally, applying heat or cold packs to the affected areas can offer temporary comfort. Over-the-counter pain relievers like acetaminophen or ibuprofen may also be effective in managing this pain. Seeking guidance from healthcare professionals who specialize in withdrawal management can provide individuals with additional strategies to cope with muscle and joint pain.
It is crucial to remember that muscle and joint pain during withdrawal is only temporary, and it will gradually diminish as the body adjusts. Seeking support from loved ones, participating in support groups, and receiving psychological care are essential steps in managing the discomfort and challenges of withdrawal. Prioritizing self-care and following a comprehensive plan for managing withdrawal symptoms are key components of a successful recovery journey.
Read our article to find out how clonidine helps with benzo withdrawal and manage the symptoms.
3. Anxiety and Restlessness
Anxiety and restlessness are common symptoms of drug withdrawal, and they result from the body adjusting to the absence of the drug it relies on. During drug use, the brain and nervous system undergo significant changes, and when the drug is removed, the body needs time to readjust.
Withdrawal can cause anxiety, which includes feelings of unease, tension, and nervousness. Restlessness can manifest as an inability to sit still, pacing, or constant movement. Despite being distressing, these symptoms are a natural part of the withdrawal process.
It is important to remember that these symptoms are temporary and will gradually subside over time as the body adjusts. Having a supportive environment and access to professional help is crucial during this process.
“Anxiety sensitivity is indirectly associated with greater likelihood of using alcohol, cigarettes, and electronic nicotine delivery systems in the past-month through anxiety symptoms,” claims a study published in the Journal o Behavioral Medicine. (Effects of anxiety sensitivity on cannabis, alcohol, and nicotine use among adolescents: evaluating pathways through anxiety, withdrawal symptoms, and coping motives, Knapp et al., 2020)
Managing anxiety and restlessness during drug withdrawal may involve a combination of medical and psychological approaches. Healthcare professionals may prescribe medications to alleviate anxiety symptoms and promote calm. Additionally, psychological support and therapy can address underlying issues contributing to anxiety and restlessness.
It is essential to seek professional help when experiencing drug withdrawal symptoms, including anxiety and restlessness. Healthcare workers can provide appropriate medical care and guidance during this challenging time. Support from friends, family, and participation in support groups can also help manage anxiety and restlessness during drug withdrawal.
4. Insomnia and Sleep Disturbances
Insomnia and sleep disturbances are common during drug withdrawal. Managing these symptoms is important to help individuals navigate the process comfortably. Here are some strategies for managing insomnia and sleep disturbances:
- Establish a bedtime routine: Create a regular sleep schedule to signal your body that it’s time to wind down. This may involve activities like taking a warm bath, reading, or practicing relaxation techniques.
- Create a sleep-friendly environment: Ensure your bedroom is cool, dark, and quiet. Use blackout curtains, earplugs, or a white noise machine to block out distractions.
- Avoid caffeine and stimulants: Don’t consume caffeine or stimulants close to bedtime, as they can interfere with sleep. Choose herbal tea or decaffeinated options instead.
- Engage in regular physical activity: Exercise regularly to regulate your sleep-wake cycle and promote better sleep. Avoid intense physical activity close to bedtime, as it may make it harder to fall asleep.
- Practice good sleep hygiene: Develop healthy sleep habits, such as avoiding electronic devices before bed, maintaining a comfortable sleep environment, and using supportive bedding.
- Try relaxation techniques: Experiment with deep breathing, meditation, or progressive muscle relaxation to calm the mind and prepare the body for sleep.
Remember, everyone’s experience with drug withdrawal is unique. It may take time to find the strategies that work best for you. If insomnia or sleep disturbances persist, consult a healthcare professional for guidance and support.
5. Depression and Mood Swings
Depression and mood swings are common withdrawal symptoms during drug withdrawal. Effective management of these symptoms is important for successful recovery. Consider the following:
- Stay connected: Maintain a supportive network of friends and family.
- Seek professional help: Consult healthcare workers or addiction specialists for tailored guidance and care.
- Psychological care: Engage in therapy or counseling to address contributing emotional factors and gain coping strategies.
- Explore holistic approaches: Incorporate practices like exercise, mindfulness, and relaxation techniques for overall well-being and reduced mood swing intensity.
Remember that the severity and duration of these symptoms vary. Work closely with healthcare professionals to create a personalized plan that addresses depression and mood swings and meets your needs and goals. With the right support, managing depression and mood swings during drug withdrawal is possible, setting the foundation for a healthier and happier life.
6. Sweating and Chills
When experiencing drug withdrawal, sweating and chills often occur as common symptoms. While these symptoms may be uncomfortable, there are effective strategies that can help manage them. Here are some tips to naturally alleviate sweating and chills during the drug withdrawal process:
- Stay Hydrated: It is important to drink plenty of fluids in order to replenish lost water. By consuming water and electrolyte-rich beverages, it is possible to regulate body temperature and prevent dehydration.
- Utilize Cool Compresses: To alleviate sweating and reduce chills, applying cool compresses or ice packs to areas such as the forehead, neck, or underarms can provide relief.
- Opt for Breathable Clothing: When dealing with sweating and chills, it is beneficial to wear loose, lightweight clothing made from natural fibers like cotton. These fabrics allow for better air circulation and help regulate body temperature.
- Adjust Room Temperature: Maintaining a comfortable room temperature can be achieved by using a fan, opening windows for fresh air, or using a heater if feeling cold.
- Practice Relaxation Techniques: Engaging in deep breathing exercises, meditation, and other relaxation techniques can help reduce anxiety and stress, minimizing sweating and chills.
- Take Warm Baths or Showers: Finding temporary relief from chills can be done by taking warm baths or showers, which helps soothe the body.
- Stay Active: Engaging in light exercises or activities promotes blood circulation and helps regulate body temperature.
- Seek Medical Guidance: If sweating and chills persist or worsen, it is important to consult a healthcare professional for evaluation and appropriate treatment.
Mary, who went through a drug withdrawal process, experienced intense sweating and chills. However, she managed to find relief by implementing the strategies mentioned above and seeking support from her healthcare provider. Over time, Mary’s symptoms gradually subsided, and she successfully navigated her drug withdrawal journey.
7. Headaches and Dizziness
The common drug withdrawal symptoms include:
- Nausea and vomiting
- Muscle and joint pain
- Anxiety and restlessness
- Insomnia and sleep disturbances
- Depression and mood swings
- Sweating and chills
- Headaches and dizziness
- Cravings
To manage headaches and dizziness during drug withdrawal, consider the following approaches:
- Medication: Certain medications, like nonsteroidal anti-inflammatory drugs (NSAIDs), can alleviate pain and discomfort.
- Hydration: Stay hydrated to prevent dehydration, which can contribute to headaches and dizziness. Drink plenty of water and electrolyte-rich fluids.
- Rest and relaxation: Take time to rest and relax. Practice deep breathing exercises, meditation, and ensure sufficient sleep for overall well-being and symptom relief.
- Healthy diet: Maintain a balanced and nutritious diet to support the body during withdrawal and alleviate symptoms. Avoid caffeine and sugary foods to prevent worsening of symptoms.
- Alternative therapies: Some individuals find relief from headaches and dizziness through alternative therapies, such as acupuncture or massage. These therapies can help alleviate tension and promote relaxation.
Consult a healthcare professional or addiction specialist for personalized guidance on managing withdrawal symptoms, including headaches and dizziness. They can provide appropriate medical care, psychological support, and tailored advice. Family and friends can also offer valuable support during this challenging time.
If you are struggling with Dextromethorphan dependence, consider reading our article on how to effectively manage Dextromethorphan withdrawal.
8. Cravings
When experiencing drug withdrawal, managing cravings can be challenging. Here are strategies to cope with cravings:
- Recognize trigger situations: Identify environments, people, or emotions that lead to cravings. By recognizing these triggers, you can better prepare to avoid or manage them.
- Distract yourself: Engage in activities that divert your attention from cravings. This can include hobbies, exercise, spending time with loved ones, or practicing relaxation techniques.
- Practice mindfulness: Utilize mindfulness techniques to observe and accept cravings without judgment. Acknowledge that cravings are temporary and remind yourself of reasons for overcoming addiction.
- Seek support: Reach out to a support system that understands your struggles and can provide guidance and encouragement. This can involve friends, family members, support groups, or healthcare professionals.
- Adopt healthy coping mechanisms: Replace drug use with healthier coping mechanisms. This can include engaging in physical activity, exploring creative outlets, or seeking professional therapy.
- Use distraction techniques: Redirect your thoughts by engaging in activities that occupy your mind. This can involve reading, listening to music, playing games, or solving puzzles.
- Maintain a healthy lifestyle: Focus on a balanced diet, regular exercise, adequate sleep, and stress management. Taking care of overall well-being can reduce cravings.
- Stay committed to recovery: Remind yourself of reasons for overcoming addiction and stay committed to your recovery journey. Visualize a future free from the impact of drugs.

Managing Drug Withdrawal Symptoms
Managing drug withdrawal symptoms is crucial for individuals seeking recovery. In this section, we will explore various approaches to effectively tackle these challenging symptoms head-on. From medical detoxification to medications for symptom relief, psychological support and therapy, as well as holistic approaches, we will uncover a range of strategies aimed at providing necessary relief and support during the withdrawal process. Let’s dive into these methods and discover how they can contribute to a successful recovery journey.
1. Medical Detoxification
Medical detoxification is an essential component in managing drug withdrawal symptoms. It is important to note several key points about medical detoxification. Firstly, the entire withdrawal process is supervised by medical professionals who ensure safety and provide immediate medical intervention if necessary.
The primary objective of medical detoxification is to alleviate the various withdrawal symptoms that may arise, including nausea, muscle pain, anxiety, insomnia, depression, and cravings. Each individual’s medical detoxification plan is tailored to their specific health conditions, substance use patterns, and medical history. If needed, symptomatic medications can be prescribed to relieve specific withdrawal symptoms and improve overall well-being during the detoxification process.
Research by scientists from Yale School of Medicine confirms that medication assisted therapy reduced the risk of withdrawal and increases the adherence to the treatment, especially for opioid addiction.
Some individuals undergo medical detoxification while staying in residential units, where they receive around-the-clock care to ensure a controlled and safe environment. Psychological care, such as counseling and therapy, is integrated into medical detoxification to address both the physical and psychological aspects of addiction and withdrawal. The support of friends and family is crucial during medical detoxification as it provides emotional support and stability.
Additionally, support groups like 12-step programs and peer support groups are highly beneficial during and after medical detoxification, offering a sense of community and ongoing support for long-term recovery.
2. Medications for Symptom Relief
When managing drug withdrawal symptoms, it is important to consider medications for symptom relief. These medications can provide relief for various symptoms experienced during withdrawal. Common medications used for symptom relief include anti-nausea medications, pain relievers, anxiolytics, sleep aids, antidepressants, antipyretics, analgesics, and craving suppressants.
Anti-nausea medications can help alleviate feelings of nausea and vomiting during withdrawal. Pain relievers such as non-steroidal anti-inflammatory drugs (NSAIDs) can reduce muscle and joint pain. Anxiolytics, such as benzodiazepines, calm the nervous system and promote relaxation. Sleep aids, including sedatives or hypnotics, can regulate sleep patterns during withdrawal. Antidepressants can stabilize mood and alleviate depressive symptoms. Antipyretics can help manage sweating and chills by reducing fever and regulating body temperature. Analgesics can alleviate headaches and dizziness. Craving suppressants like naltrexone or acamprosate can help reduce cravings and support recovery.
It is important to note that medication options may vary based on the specific drug of dependence and individual circumstances. Therefore, it is essential to consult healthcare professionals for personalized care. In addition to medications, psychological support, therapy, holistic approaches, and participation in support groups can enhance well-being and proficiency in coping with withdrawal symptoms. Always consult healthcare professionals to determine the best medication and approaches for your specific needs during drug withdrawal.
3. Psychological Support and Therapy
Psychological support and therapy are crucial for managing drug withdrawal symptoms. Effective approaches include:
- Cognitive-Behavioral Therapy (CBT): This widely used approach helps individuals identify and change negative thought patterns and behaviors associated with drug use. It also helps develop healthier coping strategies and prevent relapse.
- Individual Therapy: One-on-one sessions provide a safe and confidential space to address emotional and psychological struggles related to drug withdrawal. Therapists offer guidance, support, and personalized strategies to navigate challenges.
- Group Therapy: Connecting with others going through similar experiences in a supportive environment allows individuals to share stories, learn from one another, and gain encouragement and motivation for recovery. Psychological support and therapy play a vital role in group therapy sessions.
- Family Therapy: Involving loved ones in therapy sessions benefits both the individual in recovery and their families. It improves communication, rebuilds trust, strengthens relationships, and educates family members about addiction. Psychological support and therapy are essential components of family therapy.
- Alternative Therapies: Holistic practices like mindfulness-based techniques, art therapy, and yoga can complement traditional methods. These practices, along with psychological support and therapy, promote emotional well-being, reduce stress, and cultivate inner peace and balance.
Psychological support and therapy help individuals develop skills and mindset to overcome drug withdrawal symptoms and maintain long-term sobriety.
John, a recovering opioid addict, found solace in individual therapy during withdrawal. Through therapy, he understood the reasons behind his addiction, addressed emotional pain, and developed healthier coping mechanisms. Group therapy, which incorporates psychological support and therapy, allowed him to form meaningful connections with peers also seeking recovery. John credits psychological support and therapy for his successful journey towards sobriety.
4. Holistic Approaches
Holistic approaches are essential to effectively manage drug withdrawal symptoms and promote overall well-being. Some holistic approaches to consider include:
-
Acupuncture: By inserting thin needles into specific points on the body, it is possible to reduce cravings, anxiety, and stress associated with drug withdrawal.
-
Meditation: By incorporating meditation into daily routines, individuals can promote relaxation, reduce anxiety, and improve emotional well-being during withdrawal, claims Eric L. Garland and Matthew O. Howard in their research Mindfulness-based treatment of addiction: current state of the field and envisioning the next wave of research.
-
Yoga: The practice of yoga strengthens the body, improves flexibility, and provides inner peace and balance, which aids in coping with withdrawal symptoms.
-
Nutritional Therapy: A healthy diet supports the body’s healing process during withdrawal. Consuming nutrient-rich foods, vitamins, and supplements replenishes essential nutrients.
-
Exercise: Regular physical activity releases endorphins, alleviating withdrawal symptoms, improving mood, and promoting overall well-being.
-
Aromatherapy: The use of essential oils like lavender and chamomile reduces anxiety, improves sleep quality, and provides relaxation.
-
Massage Therapy: Massage relieves muscle tension, reduces stress, promotes relaxation, improves blood circulation, and aids in toxin removal.
By incorporating these holistic approaches with medical detoxification, medications, and psychological support, individuals undergoing drug withdrawal can effectively manage their symptoms and achieve successful recovery.
Seeking Professional Help for Drug Withdrawal
Seeking Professional Help for Drug Withdrawal greatly supports managing the challenging process of quitting drugs. Consider the following key aspects:
- Professional expertise: Consult with a healthcare professional, like a doctor or addiction specialist, for accurate diagnosis and tailored treatment.
- Medical supervision: Professional help ensures necessary monitoring of vital signs, symptom management, and medication adjustments.
- Emotional support: Professional help provides access to counseling and therapy services, addressing psychological aspects of withdrawal and offering coping strategies.
- Safe environment: Undergo withdrawal in a controlled and safe setting, such as a detoxification facility or rehabilitation center, to reduce complications and increase successful recovery.
- Access to resources: Professionals have connections to support groups, community services, and educational materials, providing guidance and support throughout withdrawal and beyond.
Remember, each individual’s withdrawal experience is unique, and professional help can cater to specific needs. Seeking professional help for drug withdrawal is a proactive step towards a healthier and drug-free life.
Pro-tip: Choose a reputable healthcare professional or treatment facility that specializes in addiction medicine and offers comprehensive support services when seeking professional help.

The Importance of Aftercare and Relapse Prevention
The significance of aftercare and relapse prevention cannot be overstated when it comes to managing the withdrawal symptoms of drugs addiction. Actively engaging in aftercare programs and strategies for relapse prevention is crucial for maintaining long-term sobriety.
- Aftercare programs: Participating in support groups or counseling is essential for maintaining recovery. These programs provide ongoing support and guidance during the challenging transition period after detoxification.
- Developing coping mechanisms: Learning healthy coping mechanisms is crucial for preventing relapse. Engaging in activities like exercise, mindfulness, or hobbies can help individuals effectively manage stress and cravings.
- Building a strong support network: Surrounding oneself with a positive support network is vital. Building relationships with individuals who understand the challenges of recovery can provide a sense of belonging and encouragement in times of temptation.
- Identifying triggers: Recognizing and avoiding triggers that may lead to relapse is essential. By identifying specific situations or environments that may increase the risk of drug use, individuals can develop strategies to minimize exposure or cope with these triggers effectively.
- Continuing therapy: Regular therapy sessions can help individuals address underlying issues that may contribute to substance abuse. Therapy not only helps individuals understand the root causes of addiction but also provides ongoing guidance and support during the recovery process.
By actively participating in aftercare programs, developing healthy coping mechanisms, building a strong support network, identifying triggers, and continuing therapy, individuals can enhance their chances of maintaining long-term sobriety and preventing relapse. The importance of aftercare and relapse prevention cannot be emphasized enough in successfully managing withdrawal symptoms and achieving lasting recovery.
Frequently Asked Questions
What are withdrawal symptoms and how do they vary?
Withdrawal symptoms are the physical and psychological effects that occur when someone stops or reduces their use of an addictive substance or behavior. These symptoms can vary depending on factors such as the type of substance/behavior, duration of use, age, physical health, mental and emotional state, and the withdrawal process used. Common effects include sleep disturbances, irritability, mood swings, depression, anxiety, aches and pains, cravings, tiredness, hallucinations, nausea, vomiting, diarrhea, sweating, shaking, and physical discomfort. Severe symptoms may also occur, especially for drugs and alcohol, and may require medical attention.
What should I do if I experience mild withdrawal symptoms?
If you experience mild withdrawal symptoms, it is important to take care of yourself and seek support from friends and family. You can also consult with a doctor, health professional, or a drug and alcohol service for guidance. It may be helpful to engage in calming practices, rest, and avoid physical exercise. Additionally, accurate information about drugs and withdrawal symptoms can help alleviate anxiety or fear. Remember that counseling should not be initiated during this stage of withdrawal.
When should I seek medical attention for withdrawal symptoms?
If you experience severe withdrawal symptoms, especially for drugs and alcohol, it is important to seek medical attention. This is particularly true when quitting addictive substances such as alcohol, GHB, benzodiazepines, or ketamine. Medical professionals can provide the necessary support, monitoring, and symptomatic treatment to ensure your safety and well-being.
What is withdrawal management and when is it necessary?
Withdrawal management (WM) refers to the medical and psychological care provided to patients experiencing withdrawal symptoms from ceasing or reducing drug use. It is necessary to assess if a patient is dependent on drugs and requires WM. WM is not meant to lead to sustained abstinence but is a first step before psychosocial treatment. It involves standard care practices such as providing a quiet and calm environment, accommodating patients away from those who have completed withdrawal, having healthcare workers available 24/7, and allowing patients to rest and engage in calming practices.
What are the recommended strategies for managing withdrawal symptoms?
Management of withdrawal symptoms involves various strategies depending on the type of dependence. For opioid dependence, pregnant women and patients commencing methadone maintenance treatment should not undergo withdrawal. Symptoms can be managed with medications such as clonidine, buprenorphine, methadone, or codeine phosphate. Benzodiazepine withdrawal symptoms can be managed by gradually decreasing the dose of benzodiazepines, while stimulant withdrawal symptoms may require hydration and offering symptomatic medications. Alcohol withdrawal can be difficult and may require medical intervention, monitoring, and symptomatic treatment. It is recommended to follow-up with appropriate treatment and support for underlying conditions to reduce the risk of relapse.
Where can I find additional resources and support for drug withdrawal?
Additional resources and support can be found through organizations such as the Alcohol and Drug Foundation, Alcoholics Anonymous, ReachOut.com, and SMART Recovery Australia. These organizations offer valuable information, guidance, and support for individuals dealing with drug withdrawal. Additionally, SAMHSA’s National Helpline (1-800-662-HELP) is a free and confidential treatment referral and information service available 24/7, 365 days a year, that can provide further assistance and connect you to local treatment facilities, support groups, and community-based organizations in your area.









