If you’re wondering “why do people get addicted to drugs?”, it boils down to changes in brain chemistry, inherited traits, and the influence of one’s environment. This article cuts through the complexities to provide you with concise and accessible insights into the mechanisms of addiction and the steps toward overcoming it.
Key Takeaways
- Drug addiction is a chronic brain disease characterized by a compulsive need to seek drugs due to altered brain chemistry and reward systems, leading to a vicious cycle of consumption, tolerance, and withdrawal that reinforces the addiction.
- Genetic factors account for approximately 40-60% of an individual’s susceptibility to addiction; however, environmental influences like peer pressure, family dynamics, and early childhood experiences also play critical roles in the development of substance use disorders.
- Effective treatment for drug addiction requires a personalized approach that addresses the co-occurrence of mental health disorders, provides a comprehensive treatment plan that includes various services, and focuses on individual barriers to recovery.
Decoding Drug Addiction: Understanding the Compulsive Need
Drug addiction, a formidable adversary, is a chronic, relapsing disease that transforms the brain and manipulates behavior, leading to an insatiable desire for addictive substances. This disorder, clinically referred to as substance use disorder, is far more than a series of bad choices or a lack of willpower. It’s a complex brain disease that hijacks the brain’s ability to make decisions, resulting in a compulsive drive to seek and use drugs, even when faced with devastating consequences. Those who are addicted to drugs struggle to overcome this powerful force and regain control of their lives.
Imagine a puppet master controlling a puppet. The puppeteer, in this case, is the addictive substance, manipulating the puppet—the person’s brain—to pursue drug seeking and consumption relentlessly. This transformation is not merely superficial; it alters the very fabric of the brain, stifling attempts to quit despite a genuine desire to do so. The National Institute on Drug Abuse aptly describes addiction as a chronic, relapsing disease characterized by compulsive seeking and use of drugs, often accompanied by harmful consequences.
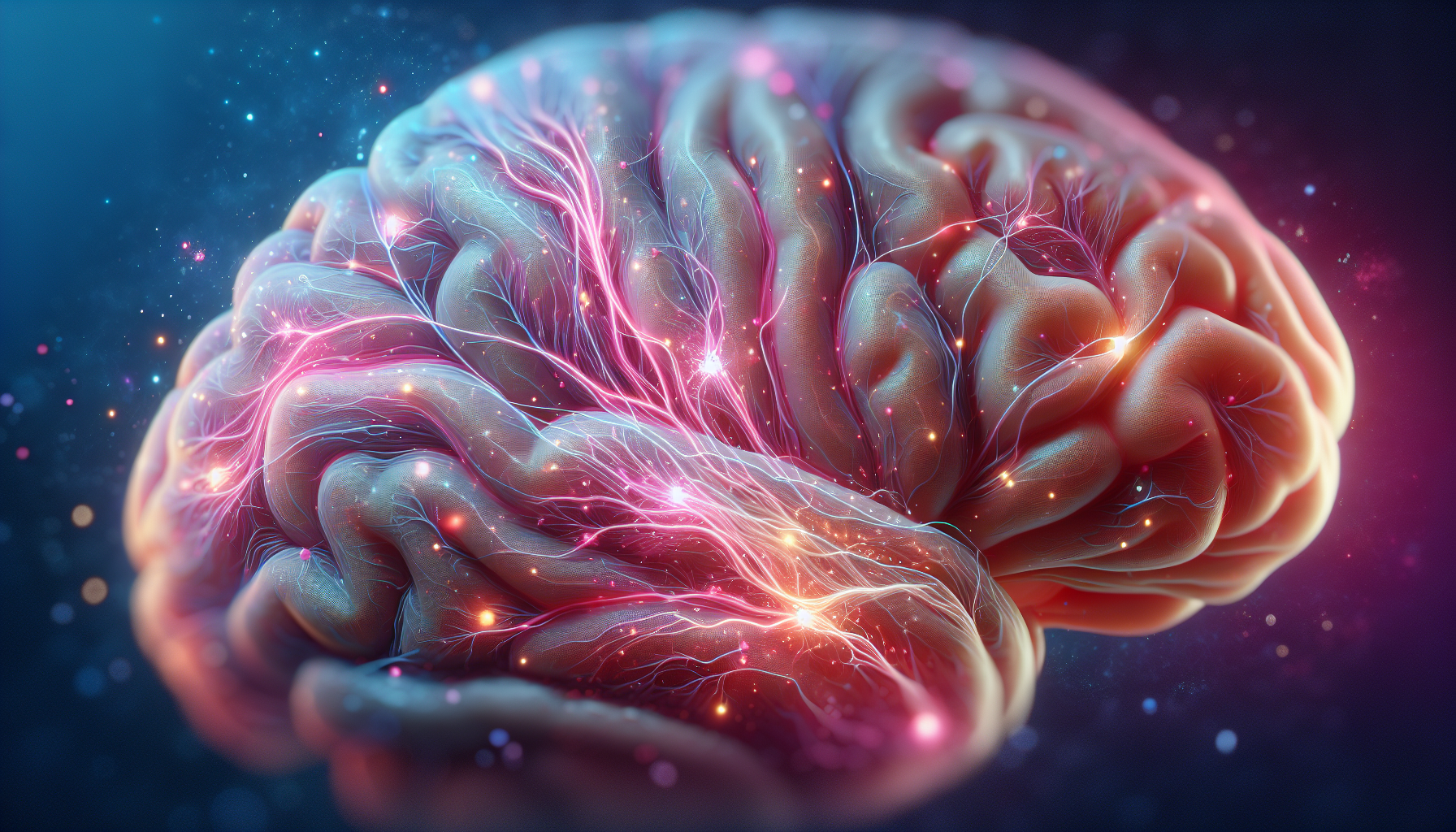
The Brain Chemistry of Addiction
At the heart of the addictive process lies a critical player—dopamine. This neurotransmitter plays a pivotal role in reinforcing drug use by signaling pleasure and strengthening neural connections for habitual behavior. Now, imagine drugs as sinister impersonators, mimicking the brain’s natural neurotransmitters and sending abnormal messages throughout the brain’s networks.
The catch with these deceptive imposters is that they produce larger surges of dopamine compared to natural rewards, thereby reinforcing the connection between drug consumption and pleasure. Over time, the brain adjusts to the presence of the drug, dulling its ability to feel pleasure from natural rewards and increasing the need for the drug to experience any pleasure. The result? A vicious cycle of increased drug consumption, tolerance, and a brain that’s been rewired to crave the very substance that’s causing harm.

The Cycle of Cravings and Relapse
We will now examine the cycle of cravings and relapse in detail. Tolerance develops as the body adapts to the presence of drugs or alcohol, necessitating higher doses for the same effect over time. Imagine running on a treadmill that’s gradually increasing in speed. As your body adjusts to the pace, you need to run faster to feel the same effect. Similarly, with drugs, the “speed” of the treadmill represents the dosage, which must be progressively increased to achieve the same high.
Withdrawal symptoms—the body’s protest against the absence of the drug—can range from discomfort to severe pain, and these symptoms often drive individuals back to drug use to alleviate the distress. This distress, coupled with the brain’s altered pleasure response and tolerance loop, substantially boosts the risk of relapse, reported to be between 40% and 60% for those in recovery. It’s a relentless cycle, one that reinforces the grip of addiction and underscores the challenge of achieving lasting recovery.
Alcohol Rehab in South Carolina
Alcohol rehab in South Carolina offers individuals struggling with alcohol addiction a supportive environment to overcome their dependence and rebuild their lives. With a range of treatment options tailored to individual needs, these facilities provide comprehensive care, including detoxification, counseling, therapy sessions, and aftercare support. Located amidst the serene landscapes of South Carolina, these rehab centers offer a peaceful setting conducive to healing and self-reflection. Highly trained and compassionate staff members guide patients through every step of their recovery journey, ensuring they receive the care and attention needed to achieve lasting sobriety. Through personalized treatment plans and a focus on holistic wellness, alcohol rehab centers in South Carolina empower individuals to break free from addiction and embrace a healthier, more fulfilling life.
The Role of Genetics and Environment in Addiction

The development of drug addiction, much like a seed sprouting, is influenced by a mix of genetic, environmental, and demographic factors. Just as not every seed sprouts, not every person exposed to drugs becomes an addict. The difference lies in the individual’s unique composition of genetic and environmental factors.
Our age, sex, and economic status are some of the demographic factors that can affect our likelihood of developing an addiction and the speed at which we might become addicted. Much like how certain seeds are more likely to sprout under specific conditions, some individuals are more susceptible to addiction under certain circumstances.
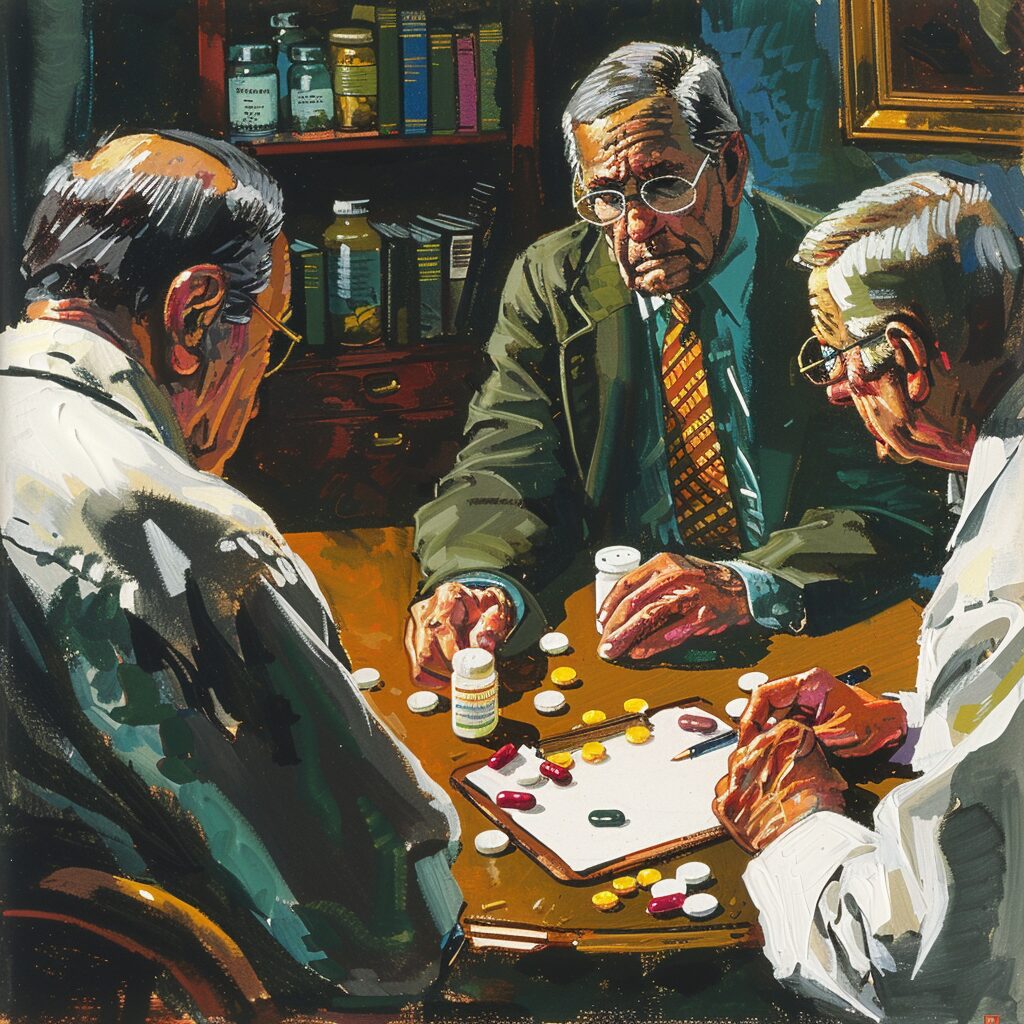
Hereditary Predispositions: Family History and Addiction
Genetics is a significant player in the game of addiction. Studies reveal that genetic factors account for approximately 40-60% of an individual’s susceptibility to addiction. One could view it as a game of genetic roulette, where birth-given genetics partially determine the odds of developing an addiction.
Genetic variation, particularly in the regulation of dopamine signaling, is central to the risk of addiction. It’s not the dopamine signaling itself, but the regulation of this signaling that’s key. In fact, researchers have identified specific single-nucleotide polymorphisms (variations in a single DNA building block) that are significantly associated with general addiction risk and specific substance disorders. The risk for addiction associated with genetic factors is observable through the correlation between parental substance use and externalizing behavior in children.
Environmental Triggers: Peer Pressure and Parental Supervision
Genetics is only half the story. Environmental factors, like the other side of a coin, play a significant role in the development of substance use disorders. Peer pressure, for instance, can be a powerful influencer, with social acceptance often tied to participating in substance use. The influence of the group can steer one’s actions, much like a current can direct a swimmer’s path.
Early childhood experiences, including the level of parental supervision and family interactions, can heavily influence the development of either healthy coping strategies or maladaptive behaviors that increase the risk of substance abuse. High levels of stress or family conflicts, such as divorce, can predispose individuals to using substances as a coping mechanism, particularly when there’s a family history of substance misuse. In essence, the environment serves as a nurturing or toxic garden where the seeds of addiction can either be stifled or encouraged to grow.
Why Do People Drink Alcohol
“Why do people drink alcohol” is a question with multifaceted answers, rooted in social, cultural, psychological, and physiological factors. At its core, alcohol consumption often serves as a means of relaxation and socialization, providing a temporary escape from stressors and inhibitions. Additionally, cultural norms and traditions play a significant role, as many societies have long-standing rituals or customs involving alcohol. Psychological factors such as peer pressure, coping mechanisms for emotional distress, or even the desire for self-expression can also influence drinking behavior. Moreover, the addictive nature of alcohol and its ability to induce euphoria or alter mood contribute to its widespread consumption. However, it’s essential to recognize that individual motivations for drinking vary greatly, and understanding these reasons can help address potential issues related to alcohol misuse and dependency.
Mental Health Disorders and Substance Abuse: A Two-Way Street

Mental health disorders and substance abuse intersect in a complex relationship, where each condition influences and exacerbates the other. Picture two rivers merging to form a powerful current. The first river represents mental disorders, and the second, substance abuse. Together, they create a formidable current that can be challenging to navigate.
Trauma, life stressors, and stress-induced epigenetic changes in gene expression are significant risk factors for drug and alcohol use. Individuals with mental health disorders, such as post traumatic stress disorder and anxiety disorders, may use substances as a means to self-medicate and deal with their symptoms. In other words, they might turn to drugs or alcohol as a way to momentarily escape the current, only to find themselves further swept away by the powerful flow of addiction. Experiences of physical and sexual abuse, including sexual abuse, can also contribute to these risk factors and the development of mental health disorders.
Co-occurring Disorders: When Drug Abuse Meets Mental Illness
When mental illness and drug abuse co-occur, it often presents challenges for diagnosis and treatment due to the interplay of overlapping and interacting symptoms. Untangling this relationship can be as complex as separating two knotted ropes. Each rope represents a disorder, and the knots are the symptoms. The task of untangling becomes more complex when the ropes are intertwined.
Understanding these interactions is critical for effective treatment. Substance use can worsen mental health disorders, and some mental health conditions can increase susceptibility to substance abuse. It’s a complex web that requires a nuanced understanding and a comprehensive treatment approach to manage effectively, underscoring the importance of personalized care in addiction treatment.
From Experimentation to Dependency: How Casual Use Becomes Addiction

The progression from casual drug use to addiction is akin to a ship gradually getting pulled into a whirlpool. It often starts with experimentation, typically in a social setting, where there’s little to no craving or dependence. This is where drug addiction begins. The ship is sailing smoothly, with the captain— the person— in control.
However, as drug use becomes regular, patterns emerge, like weekend consumption or use during periods of loneliness, which instills a mental reliance on the substance. The ship begins to circle the whirlpool, gradually losing control. By the time full addiction sets in, the ship is at the mercy of the whirlpool’s pull, characterized by an inability to feel complete without the drug and significant isolation from societal bonds.
The final stage—a crisis or the realization of the need for treatment—represents the ship’s desperate plea for rescue, necessitating professional rehabilitation services for recovery.
Preventing Addiction: Strategies That Work

Preventing addiction equates to building a protective barrier against a storm. Successful strategies, such as family therapy, school-based programs, and community efforts, can provide strong defenses against the forces of addiction. These strategies are the bricks and mortar that fortify our barrier, providing protection and resilience against the storm of addiction.
These prevention programs involving families aim to reduce substance abuse rates by tackling various aspects of life, including family relationships, education, and community norms. A well-implemented prevention program, much like a well-constructed barrier against a storm, can help individuals withstand the pull of addiction.
Educating Young Adults: The Power of Knowledge and Support
Empowering young adults with accurate information about the risks of drug use and strategies for resisting peer pressure is crucial in enabling them to make informed choices. Knowledge is power, and when it comes to addiction, this power can be transformative. Integrating drug prevention education into the standard health curriculum in schools ensures that all students receive consistent and accurate information about substance abuse.
Parental monitoring and education programs are vital in reducing adolescent drug use. Here are some reasons why:
- They set clear rules on substance use
- They engage parents in their children’s lives
- They provide the right knowledge and support to guide children towards safety and away from addiction
Community Involvement: Building Resilience Against Substance Abuse
The community plays a pivotal role in preventing addiction. Engaging community members in the development of substance abuse prevention programs ensures that initiatives are culturally relevant and more likely to be accepted and supported by the community. A community can unite to combat the threat of addiction, in the same way, it rallies to support its members in times of crisis.
Community coalitions that include various groups like schools, law enforcement, and businesses can create prevention strategies tailored to community needs. By organizing rural treatment camps, community festivals, and collaborating with local NGOs, communities can effectively raise awareness and offer treatment against substance abuse.
The community, in essence, acts as a protective shield, offering its members a safe haven from the storm of addiction.
Why Do People Abuse Alcohol
“Why do people abuse alcohol?” is a question that delves into the complexities of human behavior and psychology. There are numerous factors that contribute to alcohol abuse, including social, psychological, and biological influences. For some individuals, alcohol serves as a coping mechanism to deal with stress, anxiety, or underlying mental health issues. Additionally, environmental factors such as peer pressure and societal norms can play a significant role in influencing alcohol consumption patterns. Genetic predispositions and family history of alcoholism also contribute to an increased risk of abuse. Moreover, cultural attitudes towards alcohol and its availability can impact an individual’s likelihood of abusing it. Overall, the reasons behind alcohol abuse are multifaceted and often interconnected, making it a challenging issue to address comprehensively.
Navigating Recovery: Approaches to Successful Drug Addiction Treatment
Navigating the turbulent seas of addiction can be a daunting task. The compass guiding you through these tumultuous waters is a comprehensive drug addiction treatment plan, addressing various aspects of life beyond substance abuse itself, including:
- Family relationships
- Financial services
- Education
- Vocation
- Mental health
- Medical care
Successful addiction treatment requires a combination of services designed to address individual barriers to recovery, which may include physiological, behavioral, and social factors. It’s like having a skilled crew onboard, each member playing a vital role in navigating through the storm and maintaining the course towards recovery.
Personalized Care: Tailoring Treatment to Individual Needs
Personalized care in addiction treatment should be bespoke, like a tailored suit, designed to fit the individual perfectly. Treatment programs must take into account a person’s unique experiences, strengths, and struggles, and be tailored to address the individual reasons for substance use, which can range from:
-
seeking pleasure
-
escaping pain
-
grief
-
trauma
Just as a tailor would consider the individual’s body shape, style preferences, and the occasion for the suit, health care providers must consider the type of drug used by the individual, the context of their life, and their specific needs when crafting a personalized treatment program. With long-term care, transitional support, and aftercare planning, these personalized treatment plans cater to the specific needs and circumstances of each person in recovery.
Summary
As we conclude our exploration of drug addiction, we hope that you have gained a deeper understanding of this complex issue. We have journeyed through the biochemistry of addiction, the influence of genetics and environment, the intersection of mental health disorders and substance abuse, and the journey from casual use to full-blown addiction. We have also explored effective prevention strategies and the importance of personalized care in treatment.
Remember, addiction is not a choice or a moral failing; it is a complex disease that requires understanding, compassion, and comprehensive treatment. While the journey through addiction can be daunting, with the right knowledge, support, and treatment, recovery is achievable. Let this guide serve as a beacon of hope, illuminating the path towards understanding, prevention, and recovery.
Frequently Asked Questions
What are the 4 C’s of addiction to drugs?
The 4 C’s of addiction to drugs are craving, compulsion, control, and consequences. Understanding these components can help in addressing addiction effectively.
What causes an addictive personality?
Addictive personality can be influenced by genetics, with individuals born to parents who have had addictions being more likely to exhibit addictive traits themselves. So, genetics can play a significant role in causing an addictive personality.
What is the main purpose of addiction?
The main purpose of addiction is to alleviate severe psychological distress through the consumption of substances that stimulate the brain’s reward circuit with dopamine. This reinforcement of pleasurable but unhealthy activities leads people to repeat the behavior.
What is the cause of addiction?
Addiction is a complex condition with no single cause. Changes in brain chemistry play a significant role, as substances and certain activities affect the brain’s reward center, leading to the development of addiction.
Why is drug addiction considered a complex brain disease?
Drug addiction is considered a complex brain disease due to the significant changes it causes in the brain, affecting decision-making and leading to compulsive drug-seeking behavior. These alterations obstruct efforts to quit despite the individual’s desire to do so.