Are you or someone you care about in need of methadone for opioid addiction? It’s essential to understand who can prescribe methadone, as this is a crucial aspect of legally obtaining this medication. Navigating the tight regulations and qualifying providers is the first step. This article focuses on Opioid Treatment Programs (OTPs), certified addiction specialists, and occasionally, primary care physicians who are allowed to prescribe methadone. Learn about the specific regulations and roles that enable these providers to offer such specialized care.
Key Takeaways
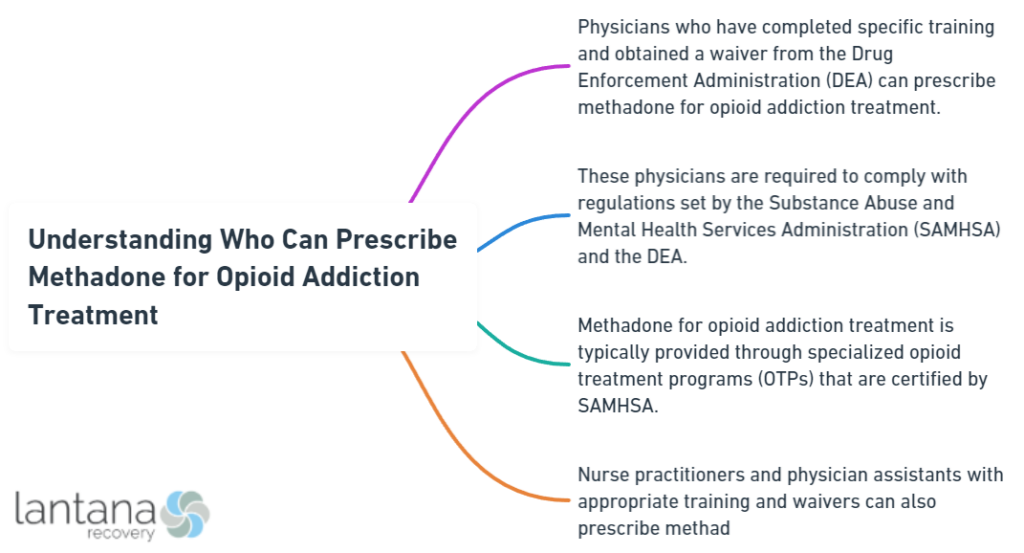
- Methadone prescribing for opioid addiction treatment is tightly regulated and generally limited to certified Opioid Treatment Programs (OTPs) and specialized addiction practitioners, with primary care providers often excluded due to intricate federal laws.
- SAMHSA and the DEA oversee the regulatory framework of methadone distribution, which requires clinic visits for treatment initiation and dosing, contrasting with the increased accessibility of buprenorphine which can be prescribed by a wider variety of healthcare professionals.
- Policy improvements like the Modernizing Opioid Treatment Access Act of 2023 and practice innovations aim to expand access to methadone maintenance treatment, amidst efforts to address persistent barriers including geographic, socioeconomic challenges, and stigma.
Navigating Methadone Prescribing Authorities

Methadone treatment represents a beacon of hope for numerous individuals battling opioid addiction. Yet, the ability to prescribe methadone is not universally granted to all healthcare practitioners. The prescribing authority is a tightly regulated privilege, entrusted to specific entities and professionals who meet stringent criteria. Understanding who can extend this crucial lifeline is the first step in comprehending the broader landscape of opioid addiction treatment.
Only a select few navigate the intricate maze of methadone prescribing: Opioid Treatment Programs (OTPs), certified addiction specialists, and occasionally, primary care providers. Each plays a distinct role within the framework of addiction medicine, bound by federal laws and regulations designed to safeguard both patients and the public from the potential risks associated with opioid medication, including the risk of opioid overdose.
The Role of Opioid Treatment Programs (OTPs) in Methadone Maintenance
Federal agencies keenly oversee Opioid Treatment Programs (OTPs), the bedrock of methadone maintenance treatment. These facilities dispense life-restoring medication to those ensnared by opioid use disorder (OUD), adhering to a strict set of regulations that govern their operation. The certification from the Substance Abuse and Mental Health Services Administration (SAMHSA) and registration with the Drug Enforcement Administration (DEA) act as the gatekeepers to this critical opioid treatment program service.
In response to the evolving landscape of public health needs, notably during the COVID-19 pandemic, OTPs have adapted their protocols to better serve patients. The advent of extended take-home doses has marked a significant shift, offering stable patients a respite from the daily visits that once defined methadone treatment. These changes, while temporary, reflect a growing recognition of the need for flexibility in addiction treatment to accommodate the diverse circumstances of those in recovery.
Addiction Specialists: Gatekeepers of Methadone Prescriptions
Addiction medicine specialists, pivotal figures in the sphere of methadone treatment, shape the recovery journey with their expertise. These highly trained professionals, often physicians with specialized knowledge in addiction psychiatry or medicine, are tasked with the complex responsibility of:
- Assessing, planning, and monitoring the methadone treatment process
- Fine-tuning the nuances of each patient’s treatment plan
- Ensuring a personalized approach that upholds safety and efficacy
It is through their clinical judgment that the methadone treatment process is guided and optimized.
The criteria that addiction specialists employ to determine patient eligibility and methadone dosage are meticulous, reflecting the gravity of their role in combating opioid addiction. With an eye for detail and a hand guided by experience, they are the sentinels who decide the appropriateness of take-home doses, a decision that balances the autonomy of the patient with the need for controlled substance management.
Clarifying the Role of Primary Care Providers
Yet, the complex world of methadone prescribing has its boundaries, often sidelining primary care providers. Despite their frontline position in healthcare, these practitioners are typically unable to prescribe methadone for OUD due to the complex web of federal regulations that specifically govern methadone dispensing. The requisite for patients to attend certified facilities for dosing, particularly in the initial treatment phase, places a barrier between primary care settings and the provision of methadone treatment.
Yet, it’s worth noting the exceptions that have surfaced during extraordinary times. The COVID-19 pandemic, for instance, saw a temporary easing of regulations that allowed for increased take-home doses, suggesting a flexibility that could, perhaps, foretell future shifts in the methadone prescribing paradigm.
Alcohol Rehab South Carolina
If you or someone you know is struggling with alcohol addiction in South Carolina, seeking professional help from reputable alcohol rehab centers is crucial. These facilities offer a range of treatment options tailored to individual needs, providing a supportive environment for recovery. In South Carolina, alcohol rehab programs often incorporate a combination of therapy, counseling, medical detoxification, and support groups to address both the physical and psychological aspects of addiction. By participating in a comprehensive alcohol rehab program, individuals can learn valuable coping skills and strategies to maintain sobriety long-term. It’s important to research and choose a reputable alcohol rehab facility in South Carolina that aligns with your specific needs and preferences to maximize the chances of successful recovery.
The Regulatory Framework Governing Methadone Prescribing

Methadone treatment is a tapestry woven with stringent regulatory threads that ensure the safe, structured distribution of this powerful medication. At the heart of this framework are the Substance Abuse and Mental Health Services Administration (SAMHSA) and the Drug Enforcement Administration (DEA), whose certifications and registrations are prerequisites for any entity aspiring to dispense methadone for opioid addiction treatment. The rigor of these regulations is borne out of necessity, reflecting the delicate balance between accessibility to treatment and prevention of opioid misuse.
Patients embarking on methadone treatment are required to navigate a regimen of daily clinic visits, a stark contrast to obtaining prescriptions through a pharmacy. This, coupled with the prohibition of telemedicine in initiating treatment, underscores the tight grip of federal law on methadone’s distribution—a grip that, thanks to recent updates, has begun to loosen slightly, allowing for some patients to receive take-home doses under specific conditions. In parallel, the DEA’s revisions have opened the door for a limited three-day supply of methadone to be dispensed, hinting at a gradual shift towards greater accessibility.
Understanding SAMHSA’s National Helpline and Resources
In the journey through the complexities of methadone treatment, the Substance Abuse and Mental Health Services Administration (SAMHSA) extends a lifeline in the form of its National Helpline. This confidential, toll-free service operates incessantly, offering guidance and treatment referral services to individuals and families ensnared by the throes of substance use disorders.
The helpline represents a beacon of support, illuminating the path to recovery with resources and information readily available in both English and Spanish, 24/7, 365 days a year.
Methadone Prescribing vs. Buprenorphine Treatment
Various therapeutic options pepper the landscape of opioid addiction treatment, with methadone and buprenorphine being the most prominent forms of opioid agonist treatment. While both serve the same noble purpose of combatting opioid use disorder, their paths diverge when it comes to prescribing protocols. To treat opioid addiction effectively, methadone, with its potent efficacy and ability to retain patients in treatment for extended periods, has historically been restricted to a narrow cadre of healthcare providers.
In stark contrast, buprenorphine has witnessed a broadening of its prescriber base, thanks to legislative changes that have eliminated the need for a special waiver, thus enabling a larger array of healthcare professionals to offer this form of substance abuse treatment. This expanded scope aims to integrate buprenorphine more fully into the healthcare system, potentially addressing treatment deserts and enhancing the reach of opioid agonist therapy.
Why Can More Providers Prescribe Buprenorphine?
The enigma of why buprenorphine can be prescribed by a more extensive array of providers than methadone is rooted in differing regulatory landscapes. Unlike methadone, buprenorphine does not necessitate the same level of oversight, allowing it to be more seamlessly integrated into general healthcare practices, thereby expanding its reach and potentially reducing disparities in treatment availability, especially in rural areas.
What is Rehab
“What is rehab?” is a common question among those seeking assistance for addiction or recovery from injury or illness. In essence, rehabilitation, often shortened to rehab, is a structured process aimed at helping individuals regain or improve their physical, mental, or social functioning. It encompasses a range of interventions tailored to address specific needs, whether they be related to substance abuse, physical injuries, or mental health challenges. Rehab programs can vary widely in their approaches, from medical detoxification and therapy sessions to vocational training and support groups. Ultimately, the goal of rehab is to empower individuals to lead healthier, more fulfilling lives by equipping them with the tools and skills necessary to overcome obstacles and thrive.
The Interprofessional Approach to Opioid Agonist Therapy
In opioid agonist therapy (OAT), a diverse range of healthcare professionals harmoniously play their respective roles in a coordinated approach to pain treatment. Nurses, in particular, are instrumental in this ensemble, offering education on the neurobiology of addiction, discussing treatment options, and fostering a supportive environment through empathic engagement. The collective efforts of this diverse team are critical in addressing not only the physical aspects of opioid dependence but also the social and emotional dimensions that underpin recovery.
Embracing cultural sensitivity and affirming care is paramount in creating inclusive treatment environments that cater to the needs of marginalized communities, such as LGBTQIA+ individuals and people living with HIV. Such an approach is essential in dismantling the barriers to methadone access and fostering trust in the treatment process.
Expanding Access to Methadone Maintenance: Policy and Practice

A blend of policy initiatives and practice innovations fuels the drive to broaden access to methadone maintenance treatment. The profound impact of methadone treatment in reducing opioid-related mortality and improving public health outcomes positions it as a vital component in the response to the opioid epidemic. The policy landscape is evolving, with the Modernizing Opioid Treatment Access Act of 2023 poised to extend the reach of methadone treatment to a broader swathe of the American populace struggling with opioid use disorder.
In tandem with policy shifts, the integration of methadone maintenance therapy into primary care settings is gaining traction. This integration promises not only to broaden access but also to enhance the comprehensive care of individuals with opioid use disorders, addressing other concurrent medical concerns. The drive to permit board-certified addiction medicine specialists to prescribe methadone in these settings is a testament to the ongoing efforts to destigmatize and democratize methadone treatment.
What is Drug Rehabilitation?
“What is drug rehabilitation?” is a question that often arises when discussing addiction treatment. Drug rehabilitation refers to the process of helping individuals recover from substance abuse disorders. It involves various interventions, therapies, and programs designed to address the physical, psychological, and social aspects of addiction. The primary goal of drug rehabilitation is to help individuals achieve sobriety and maintain it in the long term. This may include detoxification, counseling, behavioral therapies, support groups, and aftercare planning. Ultimately, drug rehabilitation aims to empower individuals to lead healthy, fulfilling lives free from the grip of addiction.
Barriers to Methadone Access and How They Affect Prescribing
Despite significant strides in methadone treatment accessibility, numerous obstacles still prevent many from receiving this lifesaving therapy. Geographic challenges loom large, with the median travel distance to methadone clinics in the United States far outpacing that of our northern neighbor, Canada, leaving those in rural regions particularly disadvantaged. Socioeconomic hurdles further exacerbate these disparities, as low-income individuals and those with inflexible work schedules or childcare responsibilities struggle to navigate the regulatory maze of treatment access.
Stigmatization casts a long shadow over the landscape of methadone access, with marginalized groups, including racial and ethnic minorities, facing formidable obstacles in their pursuit of treatment. The intertwining of stigma with racial identity, opioid use disorder, and methadone treatment fuels a cycle of mistrust and disengagement from the healthcare system. Yet, there is hope on the horizon, as policy changes like the Affordable Care Act have shown promise in diminishing these disparities and forging paths to treatment for those who have historically been left behind.
Addressing Myths About Methadone Side Effects and Use
Misconceptions and myths often cloud the path to recovery through methadone treatment, deterring individuals from pursuing or maintaining this addiction treatment. Contrary to common fears, methadone, when used as prescribed, does not elicit euphoria or cause profound sedation; instead, it stabilizes patients, allowing them to reclaim their lives from the grip of addiction. Moreover, concerns regarding organ damage or dental decay are unfounded, as methadone, with proper management and hygiene, poses no such threats.
Dispelling these myths is critical in fostering an environment where methadone is not seen as a crutch but as a legitimate therapeutic tool in the treatment of a chronic disease. Methadone treatment is not simply trading one addiction for another; rather, it is a strategic use of medication to support recovery and manage dependence, with the potential for a carefully supervised withdrawal process that mitigates the often-feared discomfort of discontinuation.
Summary
In conclusion, the journey through the maze of methadone prescribing reveals a complex interplay of regulations, responsibilities, and access challenges. The tapestry woven by OTPs, addiction specialists, and primary care providers, under the watchful eyes of SAMHSA and the DEA, serves to ensure the safe and effective delivery of methadone treatment. As we continue to confront the opioid epidemic, it is imperative that we address the barriers, debunk the myths, and embrace policy changes that expand access to this life-saving therapy.
Frequently Asked Questions
Can doctors prescribe methadone in the US?
Yes, doctors can prescribe methadone in the US, but they need to have a DEA license to do so.
Why is methadone so regulated?
Methadone is highly regulated due to its classification as a Schedule II substance and its potential for abuse, leading to severe dependence. It is also regulated by the DEA under the Controlled Substances Act.
Who can prescribe methadone Canada?
Only physicians approved by Health Canada, on recommendation from their provincial licensing body, can prescribe methadone for opioid addiction in Canada.
What are the differences between methadone and buprenorphine treatments?
In conclusion, both methadone and buprenorphine are effective treatments for opioid use disorder, with methadone typically being dispensed through specialized OTPs and buprenorphine being more widely prescribed by various healthcare providers.
What are some common myths about methadone treatment?
The common myths about methadone treatment include causing a high, severe sedation, organ damage, or being a short-term solution. In reality, when properly managed, methadone can stabilize individuals without causing euphoria and can be part of a long-term treatment plan for opioid addiction.