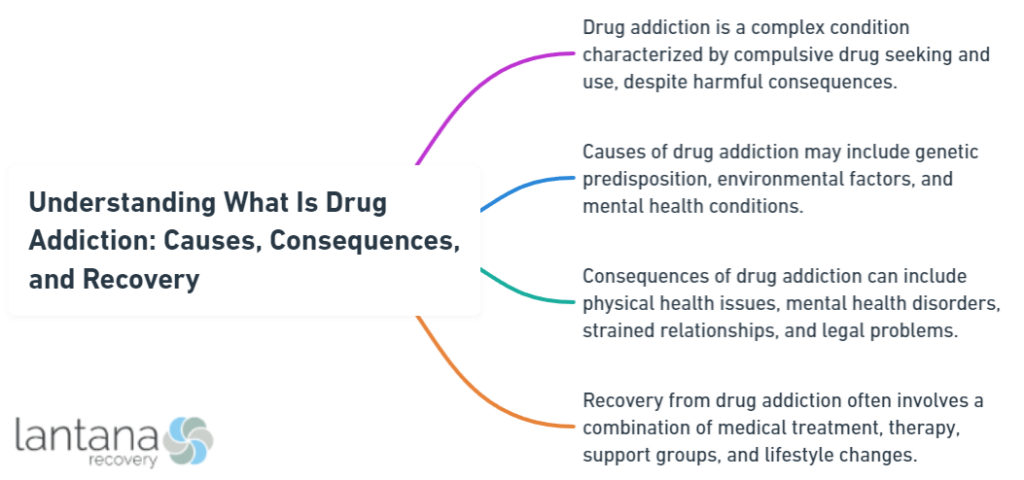
Drug addiction, or “what is drug addiction,” is the persistent urge to use drugs, regardless of harmful repercussions. Devastating lives and relationships, it is often misunderstood as a failure of will rather than a brain disorder. This article demystifies what drives an individual to addiction, how it hampers the brain’s functioning, and maps the journey towards overcoming this disorder without compromising the rich details that follow.
Key Takeaways
- Drug addiction is a chronic brain disorder characterized by compulsive drug seeking and use despite harmful effects, with genetic and environmental factors influencing susceptibility.
- Ineffective and stigmatizing misconceptions about drug addiction include the beliefs that it is a moral failing, only illegal drugs can be addictive, and addiction is a simplistic choice, disregarding the complex nature of the disorder.
- Recovery from drug addiction requires a comprehensive and personalized approach that often includes evidence-based therapies, medication-assisted treatment, support networks, and understanding the challenges of relapse and long-term management.
Exploring the Essence of Drug Addiction

Characterized by compulsive drug seeking and use despite harmful effects, drug addiction is a chronic and relapsing brain disorder that acts like a relentless predator. It masquerades as a friend, a solace, a lifeline, only to morph into a nightmare, a trap, a relentless captor. Drug use and addiction is not a simple weakness or a moral failing; it’s a severe form of addictive disorders as defined by the DSM-5, involving excessive substance-use or behavioral compulsions, often driven by the consumption of addictive drugs.
Illicit and legal substances alike can trigger this relentless predator. Alcohol, prescription medications, and illicit drugs, they all have the potential to trigger the brain’s reward circuit, leading to addiction. The overexpression of DeltaFosB in the brain, specifically in the nucleus accumbens, intensifies or attenuates addiction, creating a compulsion for drug seeking and use.
At its core, addiction hijacks the brain’s reward system. It’s a dance with danger that begins with experimentation, spirals into chronic use, and culminates in a desperate struggle to escape the clutches of tolerance and withdrawal symptoms. It’s a journey that many embark on, but few navigate successfully without help. Understanding this journey is the first step towards recovery.
The Brain’s Reward System Compromised
The dopamine-driven brain’s reward system plays a crucial role in this dangerous dance. Like a puppet master, it pulls the strings, guiding us towards pleasurable and vital survival behaviors. However, drugs can turn this master into a puppet, mimicking neurotransmitters, altering dopamine regulation, and causing artificial pleasure surges that elevate drug appeal above natural rewards.
Consistent exposure to these surges compromises the brain’s reward system, resulting in a ‘reward deficiency.’ Individuals become more sensitive to drug-related cues and less responsive to natural rewards, like a compass losing its north. The brain’s ability to revert to normal dopamine production and response to natural rewards after drug addiction can be slow and is not always fully achievable, leading to ongoing cravings.
The learned association between drug-related cues and cravings, coupled with cognitive malfunction due to alterations in brain structure and function, makes the journey even more challenging. It’s like walking a tightrope with a fickle wind, constantly threatening to knock you off balance. But understanding these changes can help regain control, turning the puppet master back into the master of the show.
The Vicious Cycle of Tolerance and Withdrawal Symptoms
The journey of addiction is further complicated by the vicious cycle of tolerance and withdrawal symptoms. Tolerance is the body’s attempt to regain equilibrium, adjusting to the presence of the substance and requiring larger amounts to achieve the original effects. It’s like a deceptive friend who keeps raising the bar, pushing you to consume more and more. The development of drug tolerance can lead to:
- Chronic pain
- Cross-tolerance
- Immune conditions
- Mental health issues
- Dependence
- Seizure disorders
- Increased risk of overdose
Conversely, the body protests through withdrawal when substance use is reduced or stops. It’s a rebellion marked by:
- aching muscles
- anxiety
- depression
- difficulty concentrating
- nausea
- sweating
The feeling that one cannot function normally without the substance, both physically and psychologically, characterizes drug dependence.
The tenacity of drug addiction is exacerbated by the cycle of tolerance and withdrawal. It’s a whirlpool that pulls individuals deeper into the abyss of addiction. The difficulty in quitting drugs is often underestimated because of the significant withdrawal challenges and physical dependence. Understanding this cycle is key to breaking free from its grip and charting a path towards recovery.
The Spectrum of Substance Use Disorders
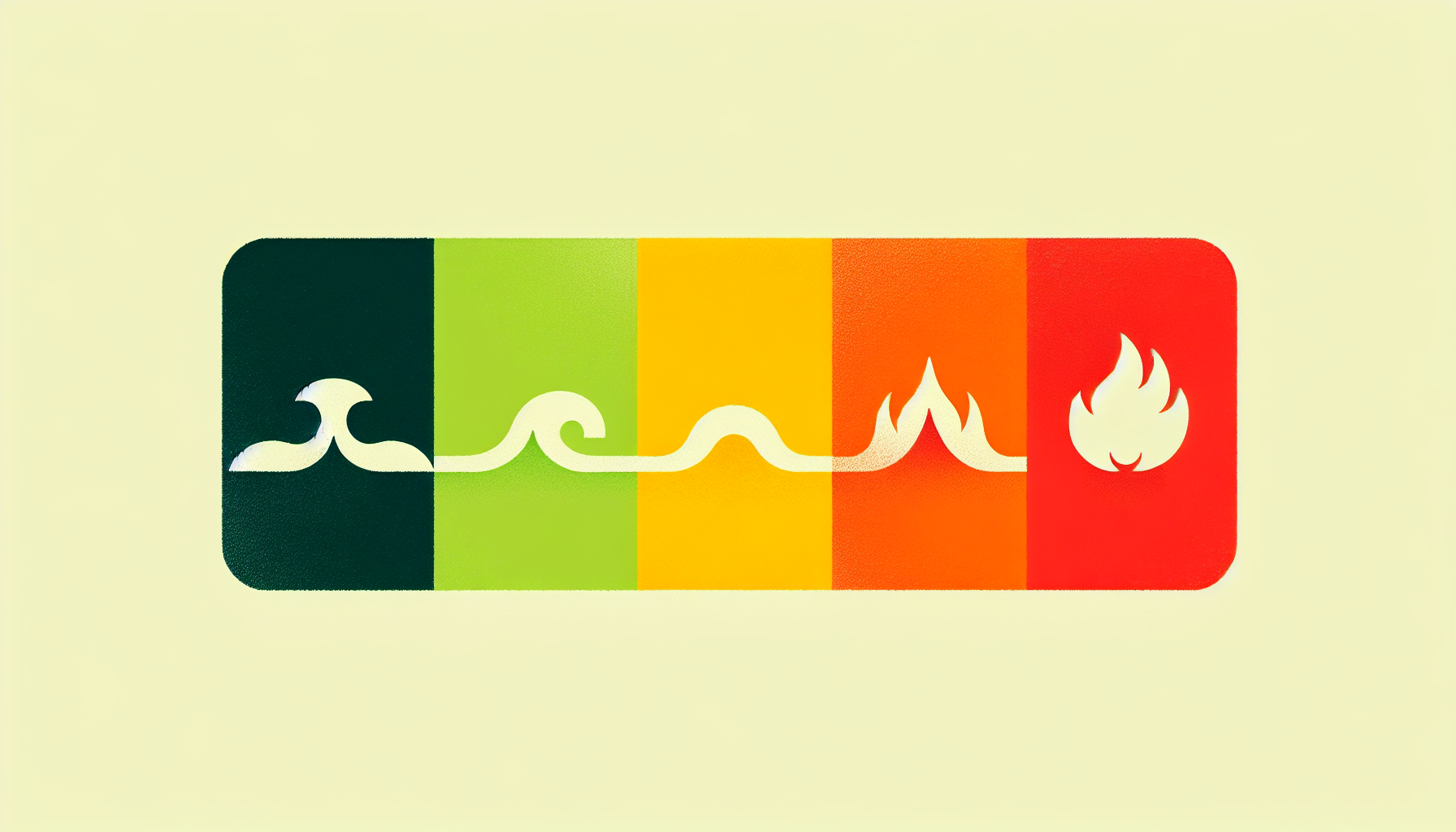
Drug addiction does not follow a one-size-fits-all model. It is part of a broader spectrum of substance use disorders, ranging from mild to severe. The DSM-5 identifies substance-related disorders linked to the use of ten specific drug categories such as alcohol, caffeine, cannabis, hallucinogens, opioids, and others. This spectrum is defined by the number of present symptoms: mild with two or three symptoms, moderate with four or five, and severe with six or more.
It’s like a scale of intensity, with each step representing a higher level of substance use disorder. The transition from initial drug experimentation to chronic abuse isn’t a sudden leap, but a gradual climb up this scale. The climb is influenced by various risk factors, including low self-control and the profound rewarding feelings drugs offer, which divert attention from normal activities to drug-taking behaviors.
The transition into drug addiction involves a psychological cycle that includes stages of binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation. Identifying the stage of an individual’s substance use disorder can guide the treatment approach, providing a tailored road map for recovery.
From Initial Drug Experimentation to Chronic Abuse
Often, the journey of drug addiction begins with just one step – initial drug use. It often involves impulsivity and acting without full consideration of consequences; this immediate rewarding feeling can lead to repeat use due to positive reinforcement. It’s like dipping your toes in the water, only to be pulled in by the undercurrent.
Continued substance use triggers neuroadaptations in the brain, transitioning from controlled, occasional use to more compulsive use, accompanied by cravings and potential for relapse. It’s a shift from casual to chronic, from choice to compulsion.
Characteristic behaviors of drug addiction include a regular need to take the drug, intense urges that disrupt other thoughts, and the necessity to consume larger amounts over time to experience the same effects. Behavioral changes signaling a transition to chronic drug abuse can include neglecting responsibilities, financial issues related to drug procurement, and persistent use despite recognizing the harms. These signs are like alarm bells, alerting us to the transition from experimentation to a full-blown substance use disorder.
Identifying Severe Substance Use Disorder
Identifying severe substance use disorder can be likened to spotting a looming storm on the horizon. It’s diagnosed according to the DSM-5 when an individual exhibits six or more criteria, which include symptoms like consuming the substance in larger amounts or for longer than intended, and a persistent desire to control or cease substance use.
Severe substance use disorder is recognizable by a pattern of compulsive drug seeking, loss of control over drug use, and intense cravings for drugs, particularly to evade withdrawal symptoms. It’s the storm at its peak, leaving havoc in its wake.
Drug dependence carries risks including:
- Changes in the brain
- Impaired judgment
- Health risks
- Overdose, which may signal the evolution into severe substance use disorder, as studied by the Institute on Drug Abuse
Recognizing these signs is the first step towards seeking help and charting a course towards recovery.
What is a Schedule 1 Drug
“What is a Schedule 1 drug?” is a question that delves into the classification system established by the Controlled Substances Act (CSA) in the United States. In this classification, drugs are categorized based on their potential for abuse and medical utility. Schedule 1 drugs are those deemed to have a high potential for abuse, no accepted medical use, and a lack of safety even under medical supervision. Examples include heroin, LSD, and ecstasy. These substances are tightly regulated by the government, making it illegal to possess, manufacture, or distribute them outside of authorized research settings. The classification of drugs into different schedules helps to guide law enforcement, healthcare professionals, and policymakers in managing substance abuse and public health concerns.
Common Misconceptions About Drug Addictions
Misconceptions about drug addiction distort reality, much like shadows. They hinder effective treatment and perpetuate stigma. One such misconception is that addiction is a moral failing rather than a health condition. However, addiction has been acknowledged in the Western world as a disease since the 19th century, challenging this misconception.
Another common misconception is that only illegal drugs cause addiction. This belief overlooks the potential for addiction that legal substances, including alcohol and prescription medications, possess. The truth is, addiction doesn’t discriminate between legal and illegal substances.
The belief that addiction is a choice is another misconception that undermines the complex nature of this disorder. While choice processes influence addiction, overcoming it is not solely a matter of willpower.
Debunking these misconceptions is crucial to fostering empathy and understanding, and facilitating effective treatment.
“Only Illegal Drugs Cause Addiction”
Believing that only illegal drugs cause addiction is akin to observing just the tip of an iceberg. Beneath the surface, there’s a vast array of substances, both legal and illegal, that can trigger addiction. Recreational substances like alcohol and marijuana, as well as prescription drugs such as opioid painkillers, all have the potential to be addictive.
Prescription medication can be misused by individuals of all age groups for non-medical reasons, often in combination with alcohol, leading to risks of drug addiction or overdose. Even individuals with a family history of addiction face increased risks when prescribed medications such as:
- opioid pain relievers
- sedatives
- tranquilizers
- stimulants for ADHD
Understanding that both legal and illegal substances can be addictive is crucial in addressing the broader issue of substance abuse. It’s a wakeup call to look beneath the surface and recognize the full extent of the addiction iceberg.
“Addiction Is a Choice”
Believing that addiction is merely a choice greatly oversimplifies this complex disorder. Gene Heyman, in ‘Addiction: A disorder of choice,’ posits that addiction results from normal choice processes and is not solely a chronic disease. The efficacy of current treatments for drug addiction, which are rooted in understanding choice processes, supports the claim that addicts can influence their substance use outcomes.
Epidemiological evidence showing that many addicts stop using drugs challenges the belief that addiction is always a lifelong affliction. However, this does not imply that overcoming addiction is simply a matter of willpower or choice. The sequence and framing of choices play a role in addiction, but they are intertwined with biological, environmental, and psychological factors.
Understanding that addiction is not a simple choice underscores the need for comprehensive treatment approaches. It calls for empathy and understanding, not judgment. It prompts us to see the struggle behind the choice and to extend a helping hand rather than a pointing finger.
Does Rehabilitation Work
The question of does rehabilitation truly works is one that encompasses a spectrum of opinions and outcomes. When considering the effectiveness of rehabilitation programs, it’s essential to recognize the diversity of individuals and the complexities of their circumstances. While some studies demonstrate promising results, showcasing reduced rates of recidivism and improved social reintegration, others suggest limitations and challenges within certain rehabilitation approaches. Factors such as the type of offense, the individual’s motivation, the quality of the rehabilitation program, and post-release support systems all play critical roles in determining the success of rehabilitation efforts. Despite varying perspectives, continual research, refinement of strategies, and holistic support systems remain vital in enhancing the efficacy of rehabilitation initiatives, ultimately striving towards successful reintegration and reduced rates of reoffending.
Recognizing the Signs of Drug Misuse
Identifying signs of drug misuse can be compared to learning map reading. It helps navigate the complex terrain of addiction, identifying potential roadblocks and detours. Individuals with a substance use disorder may not exhibit any discernible signs through appearance alone, as they can function in roles such as maintaining employment and caring for a family. It’s a deceptive disguise that conceals the struggle beneath.
However, open discussions about family history and the risks of addiction can serve as a preventive measure, particularly in families with a predisposition for substance use disorders. It’s a proactive approach to navigate the terrain of addiction, keeping an eye out for potential roadblocks.
Recognizing the signs of drug misuse is not about blaming or shaming. It’s about understanding and empathizing. It’s about knowing when to extend a hand and guide someone back onto the road to recovery.
Behavioral Indicators of Drug Use
Behavioral indicators of drug misuse act as signposts on the road leading to addiction. They signal potential detours and roadblocks, providing an opportunity to intervene and change course. Some common behavioral indicators of drug misuse include:
- Sudden disinterest in school or work
- Lack of energy
- Neglected appearance
- Secrecy about activities
- Drastic changes in relationships with family and friends
These behaviors may indicate drug misuse.
Recovering addicts who lack a support network may exhibit social withdrawal, experience depression, and potentially return to drug use to self-medicate emotional pain. It’s a detour off the path of recovery, leading back to the turbulent terrain of addiction.
Signs that a teenager or family member might be using drugs may include observable changes in behavior. These changes can be an indicator that intervention and support are needed. Recognizing these signposts is crucial to steering them back onto the road to recovery. It’s about seeing the signs, understanding what they mean, and taking action to change course.
Mental Health Red Flags
Potential drug misuse may be indicated by mental health red flags such as changes in sleep patterns, mood, and unexplained physical symptoms. They’re like warning lights on a dashboard, signaling that something is not right.
Mental health concerns related to drug use may manifest as:
- a noticeable decline in academic or work performance
- loss of interest in previously enjoyed activities
- excessive worry and fear
- extreme mood swings
- confusion
- varying levels of activity from hyperactivity to lethargy
It’s like a storm brewing beneath the surface, disrupting the calm and indicating potential trouble.
Physical symptoms without clear medical causes, such as persistent headaches or stomachaches, could also signal underlying mental health problems potentially linked to drug misuse. Recognizing these mental health red flags is crucial in navigating the road to recovery. It’s about tuning into the warning lights, understanding what they mean, and seeking help to address the underlying issues.
Alcohol Rehab South Carolina
Alcohol rehab in South Carolina offers individuals struggling with alcohol addiction a pathway to recovery in a supportive and structured environment. These facilities are equipped with professional staff and resources tailored to address the unique needs of each individual seeking treatment. Whether someone is battling alcohol dependence or facing co-occurring mental health disorders, specialized programs in South Carolina can provide comprehensive care. From detoxification to therapy sessions and aftercare planning, alcohol rehab centers in South Carolina prioritize holistic healing approaches. Additionally, many facilities offer various amenities and activities to promote physical, emotional, and spiritual well-being throughout the recovery journey. With a commitment to personalized treatment and ongoing support, alcohol rehab in South Carolina aims to empower individuals to reclaim control of their lives and achieve long-term sobriety.
The Intersection of Mental Illness and Drug Addiction

The intersection of mental illness and drug addiction can be likened to a crossroads where two arduous paths intersect. Substance abuse frequently co-occurs with mental disorders such as:
- depression
- anxiety
- ADHD
- post-traumatic stress disorder
It’s a complex interaction that exacerbates the challenges of both journeys.
Substance use can exacerbate mental health issues like depression and anxiety, leading to a bidirectional relationship where these problems feed into one another. It’s a tangled web of interconnections, where each thread pulls on the other, amplifying the difficulties.
Integrated treatment for dual diagnosis involves a combination of:
- Medication
- Counseling
- Behavioral therapies
- Support groups
It’s like having a detailed map and a compass at the crossroads, guiding the way towards recovery. Understanding this intersection is crucial to unraveling the tangled web and charting a clear path forward.
Self-Medication and Its Pitfalls
Self-medication can be compared to a double-edged sword that provides temporary relief but can cause long-term harm. Individuals may turn to substances as a means to self-medicate against painful or disturbing psychiatric symptoms. It’s a desperate attempt to ease the pain, but it often exacerbates the problem.
The use of illicit drugs, other than marijuana, increases with an unmet need for mental health care, reflecting a likelihood of self-medication. It’s a misguided attempt to fill a void, to find solace in substances when mental health care is inaccessible or inadequate.
Substance use, as a form of self-medication, can result in negative mental health outcomes such as:
- poor judgment
- paranoia
- panic attacks
- hallucinations
- delirium
It’s like a mirage in a desert, promising relief but leading to a dead end.
Recognizing and addressing the pitfalls of self-medication is crucial in navigating the journey towards recovery.
Dual Diagnosis: Treating Addiction and Mental Health Concurrently
Dual diagnosis, which represents the co-occurrence of mental health disorders and substance use disorders, can be likened to a two-sided coin. Integrated treatment, which combines substance abuse treatment with mental health services, offers the best chance of success for those suffering from drug addiction and is essential for improving patient outcomes and quality of life.
Effective implementation of integrated treatment typically requires the collaboration of healthcare professionals from both the substance abuse and mental health fields to tailor interventions suited to each individual’s need. It often involves:
- Medication
- Counseling
- Behavioral therapies
- Support groups
It’s a comprehensive approach that addresses both sides of the coin, providing a holistic approach to recovery.
Despite its benefits, integrated treatment is not universally available, with significant barriers including lack of specialized training for healthcare providers and fragmentation within the health services systems. Overcoming these barriers is crucial to ensuring that individuals with dual diagnosis receive the comprehensive care they need to navigate the road to recovery.
How Drug Addiction Begins: Environmental and Genetic Influences

The onset of drug addiction can be likened to a puzzle, where each piece symbolizes a different influence. Genetic factors account for 40–60% of the risk factors for alcoholism, indicating they significantly contribute to addiction vulnerability. It’s a genetic predisposition, like a piece of the puzzle that’s inherited.
Environmental factors that are critical in the development of addictive behavior and the transition from initial drug use to a substance use disorder include:
- Drug availability
- Family dynamics
- Peer pressure
- Cultural norms
These factors are the external pieces of the puzzle, shaping the individual’s experiences and responses.
Understanding how these genetic and environmental factors interact to influence the onset of drug addiction is key to solving the puzzle. It’s about identifying each piece, understanding how they fit together, and seeing the bigger picture.
Peer Pressure and Early Drug Use
Peer pressure can be as potent as a current, pushing individuals towards early drug use. It can manifest as direct urging from fellow peers to engage in drug use, or indirectly by creating a sense of exclusion when adolescents do not participate in certain group behaviors like smoking or drinking. It’s a force that can sweep individuals off their feet, pulling them into the turbulent waters of addiction.
Adolescents who exhibit certain personality traits, such as high sensitivity to rejection or a strong desire for peer acceptance, are more susceptible to the influence of peer pressure in their social environments. They’re like leaves caught in the current, more likely to be swept away.
Exposure to peer pressure during the critical teenage years can lead to early drug use, substantially increasing the lifetime risk of developing substance use disorders. Recognizing the power of peer pressure and providing supportive and positive influences can help individuals resist the current and stay on solid ground.
Inherited Risk and Family History
Much like invisible threads connecting individuals to their ancestors, genetics and family history play a significant role in addiction vulnerability. A family history of addiction significantly raises the risk of substance use disorders among descendants, indicating that genetic predispositions can be inherited. It’s like a genetic legacy, passed down through generations.
Family and twin studies have established a genetic link in addiction, showing that if one family member or one twin is addicted, relatives or the other twin are at a higher risk of developing addiction as well. It’s a shared heritage, a common thread that ties family members together.
For individuals with inheritable risks, the genetic predisposition to addiction can make abstaining from substance use more difficult once they begin using. Recognizing and understanding a family’s history of addiction is crucial for preventative measures, particularly as children reach adolescence when they are more susceptible to initiating substance use. It’s about acknowledging the threads of the past and weaving a new narrative for the future.
The Path to Recovery: Treating Drug Addiction
The path to recovery from drug addiction can be likened to a journey transitioning from darkness to light. It often requires personalized, intensive, and integrated treatment plans that consider the chronic nature of the disease and the high possibility of relapses. It’s a path that winds through rugged terrain, but with determination and the right support, it leads to the light of recovery.
The stages of recovery from drug addiction include:
- Abstinence: Coping with cravings and avoiding relapse
- Repair: Working on damages caused by addiction, which may include addressing past trauma
- Healing and rebuilding: Learning to navigate the path without the crutch of substance use
It’s a process of healing and rebuilding, of learning to navigate the path without the crutch of substance use.
Support systems are pivotal in the recovery process. Here are some ways to build a strong support system:
- Surround yourself with positive influences
- Seek out like-minded individuals who are also on the path to recovery
- Join support groups or attend therapy sessions
- Build a network of friends and family who are supportive of your recovery journey
By creating a strong support system, you can enrich your path to long-term sobriety.
Understanding this journey is the key to walking the path towards recovery and resilience.
Evidence-Based Therapies for Sustainable Recovery
Evidence-based therapies serve as signposts on the path to recovery from addiction. They guide individuals towards sustainable recovery, providing direction and support. Some examples of evidence-based therapies include:
- Cognitive-behavioral therapy (CBT), which helps patients recognize, avoid, and cope with situations that could lead them to use drugs and is supported by evidence to aid in the brain’s recovery from addiction.
- Dialectical behavior therapy (DBT), which focuses on teaching patients skills to manage emotions, improve relationships, and cope with stress.
- Motivational interviewing, which helps individuals explore and resolve ambivalence about changing their behavior.
- Contingency management, which provides incentives for positive behaviors and discourages drug use.
These therapies act as roadmaps, guiding individuals towards healthier thought patterns and behaviors.
Motivational interviewing aims to increase readiness to change destructive behaviors by enhancing an individual’s motivation to actively engage in treatment and plan for change. It’s like a compass, pointing individuals towards their own desire for change and motivating them to take the steps towards recovery.
Contingency management utilizes operant conditioning to encourage abstinence, providing rewards or vouchers for negative drug tests to reinforce drug-free behavior. It’s like a guiding star, providing positive reinforcement and motivating individuals to stay on the path to recovery.
Understanding these therapies is key to navigating the journey towards recovery and resilience.
Medication-Assisted Treatment (MAT)
On the journey to recovery, Medication-Assisted Treatment (MAT) serves as a lifeline. FDA-approved medications are available for treating opioid use disorders (OUD) such as buprenorphine, methadone, and naltrexone, as well as for alcohol use disorders (AUD), including acamprosate, disulfiram, and naltrexone. It’s like an anchor, providing stability in the stormy seas of addiction.
MAT medications can:
- Normalize brain chemistry
- Block the euphoric effects of drugs
- Relieve physiological cravings
- Help normalize body functions, reducing the likelihood of relapse
They’re like a lifeboat, providing support and security amidst the turbulent waters of addiction.
Combining medication with behavioral therapies can effectively treat substance use disorders, increase retention in treatment programs, prevent or reduce opioid overdose, and support sustained recovery. It’s a comprehensive approach, like a well-equipped ship navigating the journey towards recovery.
Understanding MAT is crucial in charting a course towards recovery and resilience.
Navigating Challenges: Relapse and Long-Term Management
The path to recovery from drug addiction comes with its fair share of challenges. Relapse is a common challenge in the recovery journey, presenting a high risk of returning to addictive behaviors. It’s like a detour on the path to recovery, prompting a return to old habits and patterns.
Relapse is a process that can be broken down into emotional, mental, and physical stages, each with distinct characteristics and warning signs. It’s a journey within a journey, with its own twists and turns. Understanding this process is key to navigating the path to recovery and preventing relapse.
Support networks are pivotal in the recovery process, where environmental transformations and outreach to like-minded individuals enrich the path to long-term sobriety. They’re like fellow travelers on the journey, providing companionship, support, and guidance.
Navigating these challenges is crucial to staying on the path to recovery and reaching the destination of sustained sobriety.
Understanding and Preventing Relapse
On the journey to recovery, relapse represents a fork in the road. Integrated treatment programs acknowledge that relapse may occur during recovery, necessitating preparedness by both addiction and mental health professionals to effectively manage it. It’s a pitfall on the path to recovery, but with proper understanding and preparation, it can be navigated successfully.
Relapse prevention programs utilize a variety of monitoring methods including:
- Urine drug screens
- Breathalyzers
- Skin monitors
- Saliva tests
- Hair follicle drug tests
These methods ensure early detection of substance use and act as a safety net, catching individuals before they fall back into the grips of addiction.
Understanding relapse as a process and not a failure is crucial in the journey to recovery. It’s about:
-
Recognizing the signs
-
Implementing prevention strategies
-
Knowing that even if a relapse occurs, it does not mean the end of recovery. It’s merely a detour, not a dead end.
Building a Support Network
A support network can be compared to a safety net constructed on the path to recovery. Support networks are vital for:
- Preventing relapse
- Maintaining and improving emotional, mental, and spiritual health during addiction recovery
- Providing lifelines that individuals can reach out to when the journey gets tough.
The power of fellowship in groups with a mission related to recovery can be immensely beneficial, emphasizing that individuals are not alone in their struggles. These networks provide:
- Fellowship
- Friendly observation
- An environment of understanding
- The power of sharing
- A means to respond to emergencies
They’re like lighthouses, guiding individuals through the stormy seas of addiction.
Engaging in fun activities and entertainment with a recovery-oriented network is important for maintaining a sense of normalcy and enjoyment in life. It’s about finding joy in the journey, celebrating small victories, and enjoying the company of fellow travelers.
Building a strong support network is crucial to navigating the journey towards recovery and maintaining long-term sobriety.
The Societal Impact of Drug Addiction
The societal impact of drug addiction spreads far beyond the individual, much like ripples in a pond. Drug addiction places a significant economic burden on society, accounting for nearly 6 percent of the nation’s income with costs amounting to over $532 billion annually. These costs include expenses related to:
- health care
- law enforcement
- criminal justice
- lost workplace productivity
- theft
- violence
It’s a wave of negative consequences that affects us all.
Approximately 28 percent of all deaths each year are attributable to tobacco, alcohol, or illicit drug use. The growing problem of substance abuse, particularly concerning alcohol and prescription drugs among older populations, is increasing the demand on health care systems. According to the National Institute on Drug, it’s a growing crisis, like a wave that’s building momentum.
Investing in addiction treatment is more cost-effective than the financial implications of incarceration or lost productivity; however, access to treatment is limited and not always covered by health insurance. Public policies that aim to curb drug addiction focus on discouraging use, making substances harder to obtain, and providing treatment for those struggling with addiction. Understanding the societal impact of drug addiction is crucial in creating effective strategies to manage this crisis and reduce its ripple effects.
Addressing the Opioid Epidemic and Drug Overdoses
The opioid epidemic coupled with the rise in drug overdoses is akin to a tidal wave engulfing the nation. Drug overdose deaths in the United States reached 93,331 in 2020, marking the highest number ever recorded. It’s a crisis of unprecedented proportions, leaving devastation in its wake.
The overdose crisis is now largely characterized by deaths involving illicitly manufactured synthetic opioids, such as fentanyl, and stimulants. Synthetic opioid overdose deaths, excluding methadone, have increased 103-fold from December 1999 to June 2023. It’s a rising tide, engulfing more individuals in its deadly grasp.
Naloxone is an opioid overdose prevention medication that reverses the toxic effects of overdose and is considered essential by the World Health Organization. It’s like a life raft, providing a chance at survival amidst the tidal wave of the opioid epidemic.
Addressing this crisis requires concerted efforts to raise awareness, provide access to life-saving medications, and implement effective treatment strategies.
Legal Implications and Rehabilitation Programs
Legal implications and rehabilitation programs associated with drug addiction represent the two facets of justice. On one side, drug addiction is often penalized rather than treated as a public health issue, with an emphasis on incarceration over rehabilitation. It’s a punitive approach, like a gavel delivering a harsh verdict.
On the other side, some prisons offer drug addiction treatment programs, which can include therapeutic communities, medication-assisted treatments, and educational courses on managing addiction. These programs are designed not only to treat addiction but also to provide skills and support to prevent relapse after release. It’s a rehabilitative approach, like a bridge to a second chance.
Balancing these two sides of justice is crucial in addressing the issue of drug addiction. It’s about recognizing the need for:
- justice
- compassion
- punishment
- rehabilitation
It’s about finding a balance that serves not only justice but also the individuals struggling with addiction.
Summary
The journey of understanding drug addiction is like navigating a labyrinth, filled with twists and turns, challenges and triumphs. We’ve explored the essence of addiction, its signs, its co-occurrence with mental illness, and the influences that spark its onset. We’ve looked at the path to recovery, the challenges along the way, and the societal impact of addiction. At the heart of this labyrinth, we’ve found a complex but conquerable disorder. With understanding, compassion, and effective treatment, individuals can navigate their way out of the labyrinth of addiction and into the light of recovery.
Frequently Asked Questions
What is drug addiction in simple words?
In simple terms, drug addiction is a chronic brain disease that leads to compulsive drug use despite its harmful effects. This condition requires integrated treatment and can have long-lasting effects.
What is the legal definition of a drug addiction?
Drug addiction, also known as substance use disorder, is a disease that affects a person’s brain and behavior, leading to an inability to control the use of legal or illegal drugs or medicine. It also includes substances such as alcohol, marijuana, and nicotine. The legal definition of an addict includes individuals who habitually use narcotic drugs to an extent that endangers public health, safety, or welfare, and have lost the power of self-control with reference to their addiction.
What are some common misconceptions about drug addiction?
Some common misconceptions about drug addiction are that only illegal drugs can cause addiction, and that addiction is a choice. These misconceptions oversimplify the complex nature of the disorder and can hinder effective treatment.
How does drug addiction affect the brain’s reward system?
Drug addiction alters the brain’s dopamine-driven reward system, causing artificial pleasure surges that elevate drug appeal above natural rewards and lead to a sensitivity to drug-related cues.
What are the signs of drug misuse?
If you notice sudden disinterest in school or work, neglected appearance, secrecy about activities, drastic changes in relationships, and unexplained physical symptoms like headaches or stomachaches, it could indicate potential drug misuse. It’s important to address these signs promptly to prevent further harm.