Key Takeaway:
- There is a strong link between mental illness and addiction, as individuals with mental illness are more likely to develop an addiction and vice versa.
- The contributing factors of mental illness and addiction include genetics, environmental triggers, brain chemistry, and substance abuse. Understanding these factors can help in the prevention and treatment of mental illness and addiction.
- Different forms of mental illness and addiction, such as anxiety, depression, bipolar disorder, and substance use disorders, each require their own types of treatment. Cognitive behavioral therapy, medication, and support from groups and organizations are all effective treatment options.
Are you struggling to make sense of the link between mental illness and addiction? Discover how mental illness can affect trying to break an addiction and what help is available. You don’t have to face addiction on your own.
Understanding the Link Between Mental Illness and Addiction
As someone who has struggled with both mental illness and addiction, I know firsthand how difficult it can be to untangle the complex web that ties them together. In this piece, we will explore the intricate link between these two afflictions in depth. We will start by defining exactly what we mean by mental illness and addiction, providing examples and statistics to illustrate the scope of the issue. From there, we will delve into the ways in which these two challenges are intertwined, expanding on the connections and relationships that have been identified by research and personal experience alike.

Defining Mental Illness and Addiction
Defining Mental Illness and Addiction
When it comes to mental illness and addiction, the mere mention of these two words separately can instill fear within most individuals. Now, imagine having both these problems co-existing within you? It’s a complex issue that requires careful attention and understanding.
Mental illness refers to a range of conditions that affect an individual’s mood, thinking, and behavior. These can include anxiety disorders, depression, bipolar disorder, schizophrenia, and more. Addiction refers to the compulsive use of substances or activities despite negative consequences. It is often linked to drugs or alcohol, but addiction can manifest in many other ways like gambling, sex addiction, etc.
The link between mental illness and addiction has been well established by studies over the years. The connection is bi-directional – meaning one can trigger or exacerbate the other. Individuals with mental health issues are more prone to addiction because they use substances as a coping mechanism for their problems. On the other hand, those struggling with addiction may develop mental health issues due to substance-induced damage to the brain.
It’s important to note that mental illness and addiction are not character flaws or weaknesses; it’s a disease that requires treatment just like any other medical condition. A lack of awareness and societal stigma surrounding these issues have often ended up hindering access to necessary treatments.
According to research by the National Institute on Drug Abuse (NIDA), up to 65% of individuals with substance use disorders also have at least one co-occurring psychiatric disorder. Providing proper care for individuals with such complex illnesses requires an integrative approach involving psychiatrists, psychologists, social workers, primary care physicians all working together.
I still remember my friend who was diagnosed with bipolar disorder in college had difficulty accepting her conditions leading her down a path fuelled by drug abuse where she struggled for years before finally getting help from professionals who treated her holistically for her dual diagnosis.
Stay tuned! Because, in the next section – Factors Contributing to Mental Illness and Addiction, I’ll show you how several factors contribute to the development of these two issues.
Factors Contributing to Mental Illness and Addiction
As someone who has witnessed the detrimental effects of addiction and mental illness, I know firsthand the importance of understanding the link between the two. In this section, we ll explore the various factors that contribute to the development of mental illness and addiction. We ll delve into the role of genetics in predisposing individuals to these conditions, as well as environmental triggers that can exacerbate symptoms. Additionally, we ll examine how imbalances in brain chemistry can impact mental health, and how substance abuse can further complicate the situation. With the help of expert sources and research studies, we can gain a deeper understanding of the complex relationship between mental illness and addiction.

The Role of Genetics
As humans, we all have certain traits and characteristics that are unique to each individual. These traits can be influenced by a variety of factors including genetics, environment, and lifestyle choices. In this article, we will explore one of the major contributing factors to mental illness and addiction – the role of genetics.
Genetics plays a significant role in determining an individual’s susceptibility to various mental illnesses and addiction. It is believed that certain genes can make individuals more susceptible to developing certain mental health disorders or substance abuse problems. These genes can affect various aspects of brain function such as the way the brain processes information, experiences pleasure or reward, regulates emotions, etc.
Explore more on the connection between personality disorders and addiction.
The way genetics works in relation to mental health is complex and involves numerous genetic variations interacting with each other and the environment. Some genetic variations may increase an individual’s risk for addiction while others may decrease it. Additionally, environmental factors such as stress levels, childhood trauma, exposure to drugs or alcohol can also influence how specific genetic variations affect an individual.
Recent studies suggest that genetic testing could help identify people at high risk for addiction before they develop any symptoms. This early identification could provide an opportunity for preventive measures such as counseling or support groups to reduce the likelihood of substance abuse problems later on.
It’s important to note that genetics alone cannot determine whether an individual will develop a mental illness or addiction problem. Genetics is just one piece of a larger puzzle that also includes environmental triggers and personal lifestyle choices.
As much as genetics plays a critical role in influencing our susceptibility towards different mental illnesses and addictions, there are environmental factors that shape us as well. Let’s delve into ‘Environmental Triggers’ without delay!
Environmental Triggers
Have you ever noticed how different settings and situations can impact your mood, thoughts, and behaviors? These external factors that affect our mental state are what we call ‘Environmental Triggers’. They can take various forms such as people, places, events, or sensations that cause a psychological or physiological response.
Environmental triggers work by stimulating the brain’s limbic system, which is responsible for regulating emotions and motivation. When exposed to a certain stimulus or situation repeatedly, the brain starts to associate it with a particular emotion or behavior. For instance, if someone associates socializing with anxiety and discomfort due to past experiences, they may start feeling anxious in any social environment they enter.
Interestingly enough, some environmental triggers may be unique to an individual’s experience. A person may have specific trigger points rooted in their personal history that evoke intense emotional reactions. For example, someone who has faced bullying during childhood may feel uneasy when around aggressive individuals. Conversely, someone else might enjoy the same scenario since they have positive associations associated with similar environments.
Pro Tip: Journaling is a great way to identify and keep track of environmental triggers that affect your well-being. Make a note of situations or scenarios that make you emotionally uncomfortable so that you can work towards identifying and avoiding these triggers.
The next section delves deeper into understanding how substance abuse affects the brain chemistry of individuals struggling with addiction. Keep reading to learn more about the interplay between mental illness and addiction in a fascinating manner!
Brain Chemistry and Substance Abuse
The intricate relationship between brain chemistry and substance abuse has been widely studied and discussed in the field of addiction medicine. When substances such as drugs and alcohol are introduced to the body, they interact with neurotransmitters – chemicals responsible for transmitting signals within the nervous system. This interaction alters normal communication between nerve cells, leading to changes in mood, behavior, and perception.
The reason behind this interaction lies in the fact that certain drugs mimic or alter the action of natural neurotransmitters. For example, opioids mimic naturally occurring endorphins that produce feelings of pleasure and pain relief. Stimulants such as cocaine or methamphetamine increase levels of dopamine – a chemical linked with reward processing and motivation.
However, not all substances work the same way or impact the same neurotransmitters. Psychostimulants like MDMA or ecstasy have been shown to increase serotonin release, which contributes to feelings of empathy and well-being. Similarly, hallucinogens like LSD bind to serotonin receptors causing altered perceptions and enhanced introspection.
One important aspect to consider is that substances can alter brain chemistry long-term; this means that continued use can lead to structural changes in neural circuits or even damage cells responsible for producing neurotransmitters. A few examples include alcohol-induced thiamine deficiency leading to Korsakoff’s syndrome or cannabis use during adolescence reducing gray matter volume in specific regions of the brain.
Pro Tip: Understanding how different substances affect brain chemistry can help us identify the root causes of an individual’s addiction problem – a key step towards targeted treatment plans.
So you want to know more about Mental Illness and Addiction? Brace yourself because it’s quite an intricate dance between nature vs. nurture, social stigma vs biomedical approaches, comorbidities, gene-environment interactions…
Different Forms of Mental Illness and Addiction
When it comes to mental illness and addiction, there are many different types that can impact individuals in a variety of ways. In this part of the article, we ll be taking a closer look at the link between different forms of mental illness and addiction. Specifically, we ll be examining the relationship between anxiety, depression, and bipolar disorder and substance use disorders and addiction.
Mental health is a pressing concern in modern society, with 1 in 5 people in the United States experiencing mental illness per year (National Alliance on Mental Illness). Understanding the potential connections between different types of mental illness and addiction is crucial in order to provide effective care and support.

Examining Anxiety, Depression, and Bipolar Disorder
Mental illness is a subject that requires more attention than it currently receives. The three most common forms of mental disorders are anxiety, depression and bipolar disorder. These conditions can impact a person’s thoughts, feelings, and behaviors in various ways.
Examining anxiety, depression, and bipolar disorder allows us to understand how these conditions develop and the symptoms they produce. Anxiety disorder is characterized by a persistent feeling of worry, tension or nervousness about everyday situations or events. Depression is a prolonged feeling of sadness or hopelessness which negatively impacts an individual’s mood, thinking and daily life activities. Individuals suffering from bipolar disorder experience large swings in mood from extreme highs to lows or vice versa.
It has been discovered that various factors such as genetic predisposition, environmental stressors, brain chemistry imbalances etc., play a role in the development of these mental conditions. For instance, individuals with family members who suffer from depression are likely to have depression compared to those who don’t have similar medical history.
Check out the connection between bipolar disorder and addiction to gain a better understanding of the link between mental illness and addiction.
The effective treatment of these illnesses relies heavily on awareness and understanding the causes behind them. Knowing the symptoms and seeking medical help promptly makes all the difference for someone going through any of these illnesses.
If you or anyone you know experiences any symptoms related to anxiety, depression or bipolar disorder then taking prompt medical action is highly recommended. Chronic emotional pain can lead to torment that worsens over time due to its nature being persistent and intense. It is important to understand the connection between depression and substance abuse as well to get a better grasp of the situation.
As I journey forward into exploring further mental health issues in this article series in later sections like Substance Use Disorders and Addiction – chances are high that many of us may find ourselves fighting one form of addiction or another at some point in our lives even when we try hard not to fall victim to it.
Substance Use Disorders and Addiction
Substance use disorders and addiction are complex issues that affect millions of people worldwide. These conditions can have a significant impact on a person’s life, relationships, and mental health. Substance use disorders occur when someone continues to use drugs or alcohol despite experiencing negative consequences such as legal, financial, or health-related problems. Addiction refers to the compulsive behavior of seeking out drugs or alcohol despite these harmful outcomes.
Substance use disorders and addiction work by hijacking the brain’s reward system. When we engage in pleasurable activities such as eating, exercising, or spending time with loved ones, our brain releases a chemical called dopamine that reinforces the behavior. Drugs and alcohol also trigger this release of dopamine but at much higher levels, which can cause changes in how the brain functions over time. This can lead to a cycle of craving and compulsive drug-seeking behavior.
Although genetics play a role in who is more susceptible to developing substance use disorders and addiction, environmental factors such as stress, trauma, and peer pressure can also contribute. Substance use disorders and addiction can lead to serious physical and mental health problems if left untreated. It is essential to seek professional help if you suspect you or someone you know may be struggling with these issues.
One notable figure in the history of addiction is Bill Wilson, co-founder of Alcoholics Anonymous (AA). Wilson struggled with alcoholism for many years before achieving sobriety and then dedicating his life to helping others fight addiction through AA. His personal story has inspired millions of people around the world to seek help for their own struggles with substances.
As I delved into understanding substance use disorders and addiction further, I realized that treatment options for those dealing with these issues are numerous but often underutilized or stigmatized. From therapy to medication-assisted treatments to support groups like AA, there is no one-size-fits-all approach when it comes to recovery from substance use disorders and addiction. In my next segment, I’ll explore some of the many ways professionals are working to help individuals overcome these challenges and lead healthy, fulfilling lives.
Treatment Options for Mental Illness and Addiction
As someone who has experienced both addiction and mental illness, I know firsthand how intertwined these two issues can be. That s why finding an effective treatment that addresses both concerns simultaneously is crucial for lasting recovery. In this part of the article, I ll be discussing some of the most effective treatment options for individuals dealing with mental illness and addiction. We ll explore the benefits of Cognitive Behavioral Therapy, how medication can help manage symptoms, and the importance of seeking support through groups and organizations. These treatments have been shown to greatly improve the chances of long-term recovery and offer a pathway toward healing and hope.
Cognitive Behavioral Therapy and its Benefits
Cognitive Behavioral Therapy and its Benefits
Cognitive-behavioral therapy, commonly known as CBT, is a type of talk therapy that helps you to identify negative behavior patterns and change them. This approach involves a combination of cognitive and behavioral techniques that help you understand how your thoughts, feelings, and behaviors are interconnected. It can be an effective form of treatment for mental health disorders and addictions.
CBT works on the premise that the way we think about situations affects our emotions and behaviors. By changing distorted thinking patterns such as negative self-talk or irrational beliefs, individuals can learn to manage their emotions more effectively. Additionally, changing behaviors such as avoiding triggers or engaging in activities that promote wellness can also have a positive impact on mental health.
Some benefits of CBT include:
- Improved mood
- Increased self-awareness
- Enhanced problem-solving skills
- Reduced stress levels
Research has shown that CBT is an evidence-based approach with high success rates for treating:
- anxiety disorders
- depression
- post-traumatic stress disorder (PTSD)
- substance abuse disorders, and
- eating disorders.
Interestingly enough, CBT was originally developed for use with depression but has expanded to various other mental health issues over time. The National Institute of Mental Health considers it one of the most promising forms of psychotherapy available today.
Pro Tip: Consider seeking out therapists who have experience using cognitive-behavioral techniques or enrolling in a CBT-based program to get the most out of this approach.
Feeling better already? Buckle up because the next section covers medication as a method of managing symptoms – let’s see if popping pills is always the best option!
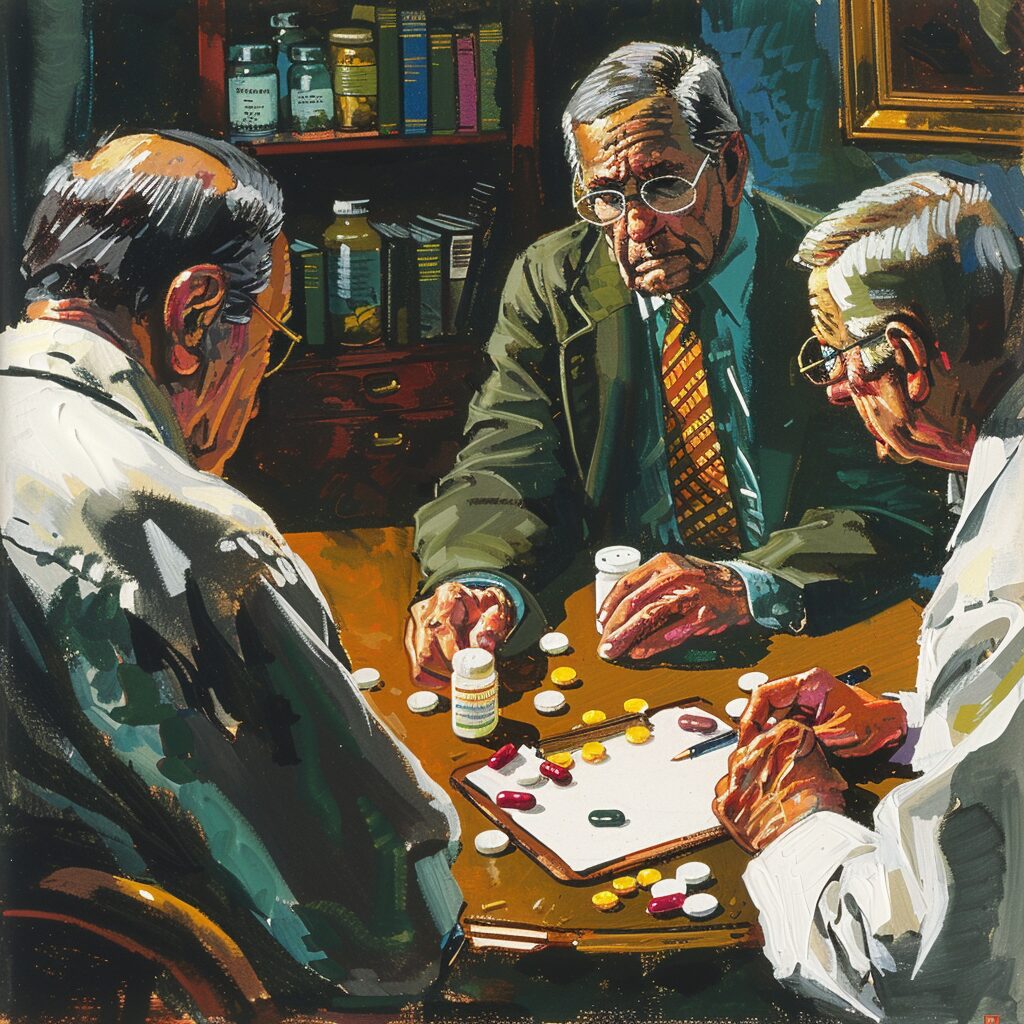
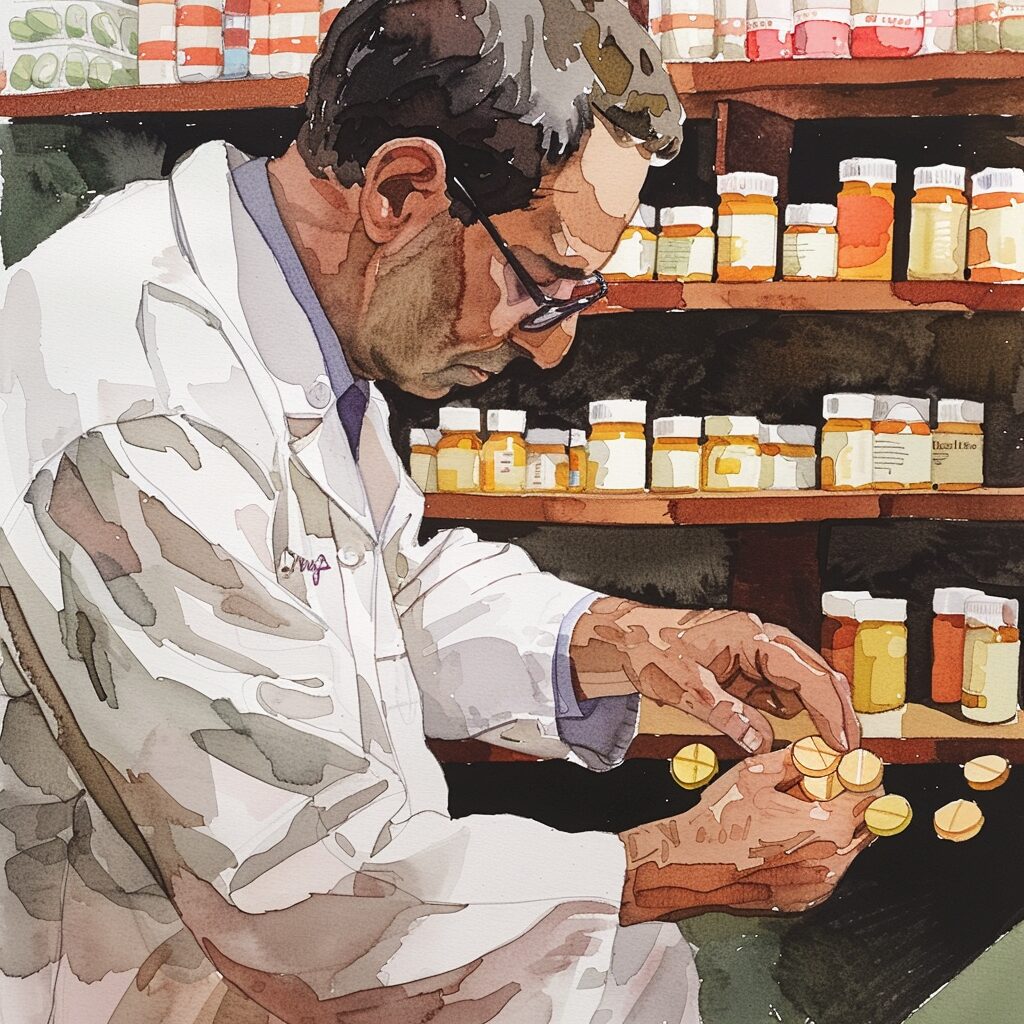
Medication as a Method of Managing Symptoms
Managing mental illness and addiction is a complex issue that requires a highly individualized approach that considers each person’s unique experiences, lifestyle factors, and mental health history. Medication is just one method of managing symptoms, but it can be an effective tool for many individuals in achieving stability and reducing symptoms.
Medication works by altering the chemistry of the brain to regulate mood, emotions, and behavior. It can address chemical imbalances in the brain that contribute to symptoms of mental illness and addiction, such as depression or anxiety. Some medications work by increasing the availability of neurotransmitters like serotonin or dopamine, while others decrease the activity of certain parts of the brain associated with negative emotions.
While medication can be very beneficial, it should not be relied upon as the only treatment option for mental illnesses or addiction. It is important to incorporate other methods alongside medication, such as therapy, support groups, and lifestyle changes. Additionally, finding the right medication often involves a trial-and-error process to determine which medication works best with minimal side effects.
It is important to note that each person’s experience with medication will be different – what works well for one individual may not work for another due to differences in genetics or metabolic processes. It is also critical to work closely with a healthcare provider when starting any new medication regimen to monitor for potential side effects or interactions with other medications.
In addition to seeking professional help when considering medication options, there are some tips that can help make taking medications easier. For example: setting reminders on your phone or keeping a pillbox can help ensure you take your medication at consistent times; tracking your moods or symptoms daily can provide insight into whether or not your prescribed dose is working effectively; and communicating openly and honestly with your doctor about any concerns you have regarding side effects.
So if you’re considering using medication as a method of managing symptoms related to mental illness or addiction, know that it can be an effective tool when used correctly and in conjunction with other treatment methods. However, it’s important to remember that it’s a highly individualized decision that requires professional guidance and ongoing evaluation.
Next up: have you considered seeking support through groups and organizations?
Seeking Support Through Groups and Organizations
Many people who are struggling with mental illness and addiction often feel isolated, misunderstood and helpless. Seeking support through groups and organizations is one way to connect with others who share similar experiences and receive assistance in navigating the challenges of mental illness and addiction.
Firstly, joining a support group can provide a sense of belonging, which is vital for recovery. People in groups come together to share experiences, discuss coping techniques, offer mutual support and validate each other’s feelings. Support groups could be located virtually or physically.
Secondly, there are many organizations that exist to provide resources, education and advocacy for those experiencing mental illness and addiction. These organizations often have hotlines that individuals can call if they need help or guidance. Some examples of such organizations include the National Alliance on Mental Illness (NAMI), the Substance Abuse and Mental Health Services Administration (SAMHSA) among many others.
Thirdly, participating in group therapy sessions may help people open up about their issues in a safe environment while also benefiting from peer feedback. Therapists can offer valuable insights into how mental illness/ addiction impacts an individual’s life as well as provide tools to manage symptoms.
Lastly, it is crucial to find the right kind of group support or organization type for oneself – age-appropriate groups may be more appropriate for teenagers with anxiety disorders while gender-based rehabilitation facilities would be required for women dealing with addiction issues.
If you’re struggling with anxiety and addiction, it’s important to understand the connection between the two. Seeking support from tested support networks near or far can help you on your recovery journey. Learn more about the connection between anxiety and addiction.
Next Up: The Blueprint for Preventing Mental Illness and Addiction is simpler than you think!
Preventing Mental Illness and Addiction
As someone who has witnessed the destructive power of addiction and the toll that mental illness can take, preventing these issues is of the utmost importance to me. In this section, we will discuss ways to prevent mental illness and addiction, with a focus on practical tips that anyone can implement in their daily lives.
First, we ll explore stress management and coping techniques, which have been proven to mitigate the risk of both mental illness and addiction. We ll also discuss how adopting healthy lifestyle habits can improve overall well-being and address underlying issues that may contribute to addiction and mental illness.
Finally, we ll delve into the importance of identifying symptoms early and seeking early intervention, which can make all the difference in preventing the devastating consequences of these conditions.

Stress Management and Coping Techniques
Stress management and coping techniques are an essential part of preventing mental illness and addiction. These techniques include various methods that help individuals manage stress levels, reduce the impact of stressful events, and engage in healthy behaviors that promote mental wellness.
These techniques work by helping individuals identify the sources of stress in their lives and providing them with skills to manage these sources more effectively. By learning to recognize triggers, set boundaries, practice self-care, and communicate effectively, individuals can avoid feeling overwhelmed by stressors they face on a daily basis.
Additionally, stress management and coping techniques also promote physical health by reducing tension in muscles and promoting relaxation. Practicing these techniques regularly can also prevent the development of anxiety disorders or depression.
One valuable technique for stress management is mindfulness meditation, which involves focusing on the present moment without judgment or distraction. Another powerful tool is cognitive-behavioral therapy (CBT), which helps individuals to identify negative thought patterns and replace them with more positive ones.
So if you want to take control of your life stress-free by avoiding anxiety disorders or depression along with substance abuse disorder (addiction), it’s time to adopt healthy habits today! Don’t let anything hold you back from achieving success start practicing mindfulness, CBT or any other form of relaxation and remain mentally healthy always!
As we move towards adopting healthy lifestyle habits for long-term success, I urge you not to miss out on tips that will transform your life forever. Trust me; it’s worth it!
Adopting Healthy Lifestyle Habits
Adopting healthy lifestyle habits involves incorporating positive habits into your daily routine that promote overall physical and mental wellbeing. This approach aims to prevent the onset or progression of mental illnesses and addiction by improving our daily choices and behaviours.
Adopting healthy lifestyle habits works by reducing risk factors associated with mental illnesses and addiction. Our daily choices can affect our brain chemistry, physical health, and emotional stability. By choosing to live a healthier lifestyle, we reduce our exposure to harmful substances, improve our mood and cognitive functioning, and strengthen emotional resilience.
Healthy lifestyle habits include practices such as regular exercise, healthy eating, adequate sleep, stress management, social connection, mindfulness practices, and abstaining from harmful drugs or alcohol. These healthy behaviours can help decrease inflammation in the body and brain which is known to be a contributing factor in many mental illnesses.
Research suggests that adopting healthy lifestyle habits can significantly reduce the likelihood of developing conditions such as anxiety disorders, depression, bipolar disorder, schizophrenia, substance abuse disorders, among others. Engaging in these activities proactively may even increase feelings of self-worth which guards against addiction progression or onset for susceptible individuals.
To ensure a life free from debilitating conditions like addiction or mental illness; it’s important to start incorporating healthy behaviours into your routine now! Don’t wait until tomorrow to start making changes; begin today before FOMO sets-in! Remember: every small step you take towards living healthier can help protect your mind-body-spirit for years to come.
Identifying Symptoms Early for Early Intervention
Identifying Symptoms Early for Early Intervention is a crucial step in preventing and combating mental illness and addiction. It involves recognizing the warning signs of these issues early on, before they become too severe or develop into a chronic condition. By detecting symptoms early, healthcare professionals can provide timely intervention and support that may prevent the onset of more serious conditions.
Early identification of symptoms relies on knowledge and awareness of the various warning signs associated with mental health concerns and addiction. This involves understanding the physical, emotional, and behavioral indicators that suggest an individual may be struggling with their mental health. Some common warning signs include changes in mood, decreased energy levels, increased substance use, and social withdrawal. Identifying these symptoms early can allow for prompt intervention that may minimize the impact of these conditions.
In addition to awareness of warning signs, identifying symptoms early for early intervention requires accurate diagnosis by qualified professionals. Mental health concerns are complex and diverse in nature, making an accurate diagnosis vital for effective treatment. Therefore, proper assessment tools ought to be used to ensure accurate evaluation of patients’ conditions.
Early identification also improves the chances of alternative non-medical solutions being prescribed as a first line treatment which ultimately reduces the rates at which people resort to hospitalization or involve costly psychotherapy sessions.
Upon my late grandma’s death anniversary recently sparked memories about her long struggle with clinical depression during her lifetime which worsened until it became full blown dementia before she passed away quietly in her sleep few years ago without realizing how much she had lost herself over time thereby shattering lifelong bonds with family members who didn’t understand how systematically depression silently ate into grandma s life yearningly aided by feigned normalcy when everyone once thought Grandma was okay. If only we knew earlier what some flags were: subtle changes in mood swings which oscillated between low/not good/deep sadness accompanied by dis-interest in leisure activities like cooking; irritability; feelings drained as if someone turned the energy off, sleep and appetite changes which over span of time had a strong impact on her overall health; increased alcohol consumption when she could lay her hands on some (and that wasn’t quite common for someone brought up with strict Christian values).
Through this unfortunate incidence, I learned how early detection of the signs and symptoms can help not only to mitigate extreme emotional distress, but also allow families to understand more about what their loved ones may be going through emotionally. Early intervention for mental illness and addiction is therefore crucial in order to ensure adequate support is provided before these conditions escalate into something much more severe.
Five Facts About Understanding the Link Between Mental Illness and Addiction:
- People with mental illness are more likely to develop substance abuse disorders than those without mental illness. (Source: National Institute on Drug Abuse)
- Substance abuse can worsen symptoms of mental illness and increase risk of relapse. (Source: Substance Abuse and Mental Health Services Administration)
- Dual diagnosis treatment, addressing both mental illness and substance abuse, is the most effective approach to treatment. (Source: Psychiatry Advisor)
- Common mental illnesses linked to addiction include depression, anxiety disorders, and bipolar disorder. (Source: HelpGuide)
- Early intervention and treatment can improve outcomes for those with co-occurring mental illness and addiction. (Source: American Psychiatric Association)
FAQs about Understanding The Link Between Mental Illness And Addiction
What is the link between mental illness and addiction?
The link between mental illness and addiction often coexist, with individuals who have one being at a higher risk of developing the other. Mental health conditions like depression and anxiety may drive individuals to self-medicate with drugs or alcohol, leading to addiction. Conversely, substance abuse may alter brain chemistry and worsen underlying mental health issues.
How common is the co-occurrence of mental illness and addiction?
The co-occurrence of mental illness and addiction is quite common between the two health conditions. About half of the individuals with a severe mental health condition also have a substance use disorder. Moreover, around 20% of people who have an addiction to drugs or alcohol have a mental health disorder.
Which mental health conditions are commonly linked to addiction?
These are the mental health conditions that are frequently linked to addiction. These include anxiety disorders, depression, bipolar disorder, schizophrenia, and post-traumatic stress disorder (PTSD).
What are the treatment options for co-occurring mental health and addiction disorders?
The treatment options for co-occurring mental health and addiction disorders usually involve a combination of behavioral therapies, medications, and support groups. To be most effective, treatment needs to address both disorders simultaneously. A mental health professional can determine the right treatment plan for individuals with co-occurring conditions.
Can someone fully recover from co-occurring mental health and addiction disorders?
Yes, some can fully recover from co-occurring mental and addiction disorders. With the right treatment, many individuals with co-occurring disorders can achieve sustainable recovery. It is important to seek professional help and support to achieve recovery..
Does relapse occur in co-occurring mental health and addiction disorders?
Relapse occurs in co-occurring mental health and addiction disorders and is commonly a challenging treatment. Those with addiction may experience triggers that lead to substance use, while those with a mental health disorder may experience setbacks in treatment or an exacerbation of symptoms. However, relapse should not be viewed as a failure but rather as a sign that treatment needs to be adjusted or reevaluated.