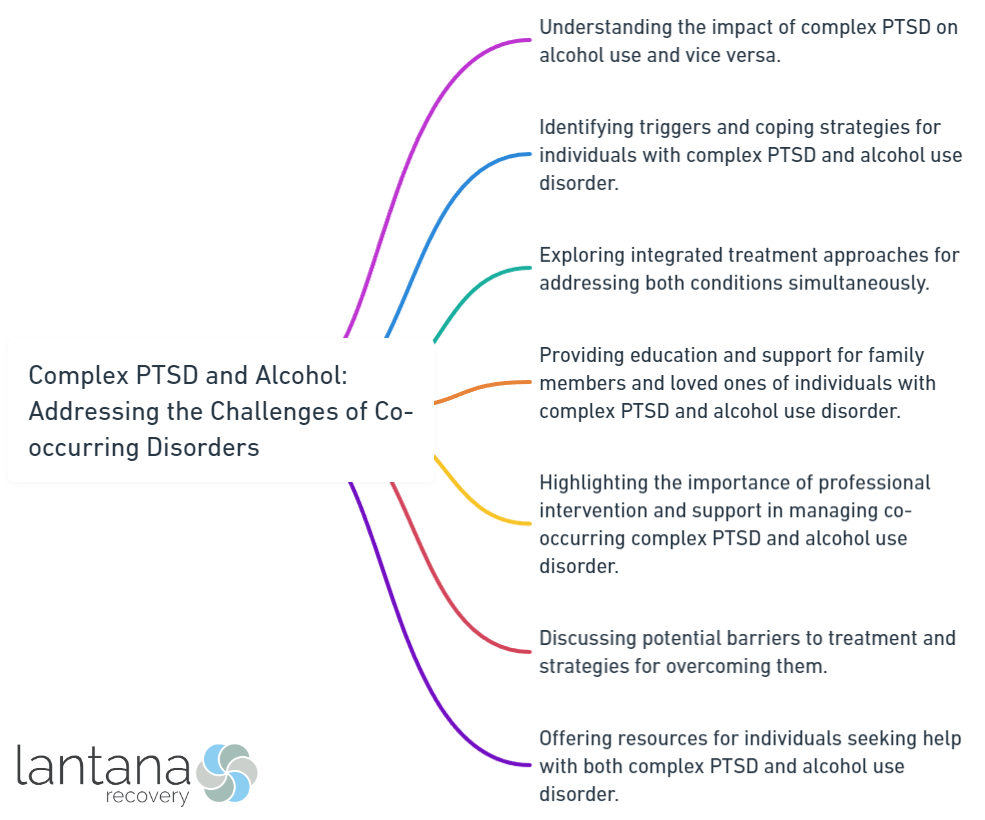
Complex PTSD (Post-Traumatic Stress Disorder) and Alcohol Use Disorder (AUD) are two challenging mental health conditions that often co-occur, presenting unique difficulties for individuals affected by both. Understanding the complexities of these disorders and addressing their co-occurrence is crucial for effective treatment and recovery. In order to comprehend the challenges posed by co-occurring Complex PTSD and AUD, it is important to first understand each disorder individually. Complex PTSD is a condition that arises from prolonged exposure to traumatic events, often in the context of interpersonal relationships. It is characterized by symptoms such as emotional dysregulation, disturbed self-perception, and difficulties in interpersonal relationships. On the other hand, AUD is a chronic condition defined by the problematic consumption of alcohol, leading to negative consequences on physical, psychological, and social levels. It manifests as a range of symptoms, including cravings, loss of control, and withdrawal symptoms. The co-occurrence of Complex PTSD and AUD is not uncommon. According to research, individuals with Complex PTSD are at a significantly higher risk for developing AUD compared to those without PTSD. The presence of co-occurring disorders exacerbates symptoms and often leads to poorer outcomes in terms of mental health and overall functioning. Addressing the challenges of co-occurring Complex PTSD and AUD requires a comprehensive and integrated approach. However, several barriers exist that hinder effective treatment, such as stigma, lack of awareness, and limited access to specialized resources. The unique treatment considerations for individuals with co-occurring disorders, such as the need for trauma-focused therapy and addressing underlying trauma while managing substance use, further complicate the process. Integrated treatment programs that combine evidence-based therapies for both Complex PTSD and AUD have shown promising results. Trauma-focused therapy aims to process and heal traumatic memories, while substance abuse treatment focuses on developing healthy coping strategies and preventing relapse. These approaches should be combined with a strong support system, self-care practices, and relapse prevention techniques to enhance recovery outcomes. By understanding the challenges, implementing evidence-based treatments, and providing ongoing support, individuals with co-occurring Complex PTSD and AUD can achieve lasting recovery and improved quality of life.
Understanding Complex PTSD
Complex PTSD, or Complex Post-Traumatic Stress Disorder, is a psychological condition that develops from prolonged trauma or multiple traumatic events. It differs from traditional PTSD as it involves ongoing trauma and affects relationships and self-perception. Understanding Complex PTSD is crucial for recognizing symptoms and providing appropriate support.
One aspect to consider is the impact of childhood trauma on the development of Complex PTSD. Research suggests that traumatic experiences during childhood, such as abuse or neglect, greatly contribute to later development of this condition. It is important to acknowledge the lasting effects of childhood trauma and understand how it shapes experiences and behavior.
Another important factor is the range of symptoms experienced by individuals with Complex PTSD. These symptoms include difficulties regulating emotions, disturbances in self-esteem, and negative self-perception. Similar to traditional PTSD, flashbacks, nightmares, and hypervigilance may occur, but individuals with Complex PTSD may also experience more severe dissociation and relationship difficulties.
Understanding Complex PTSD also involves recognizing the importance of trauma-informed care. This approach emphasizes creating a safe and supportive environment for individuals with trauma histories. It involves acknowledging the impact of trauma, promoting empowerment and choice, and avoiding retraumatization.
Fact: Trauma-exposed individuals are at a much higher risk of developing PTSD that the rest of the population. For example, the rate of PTSD among military veterans is almost 14% almost half than regular population i.e. 8%.
What is Complex PTSD?
Complex PTSD, short for complex post-traumatic stress disorder, is a psychological condition that arises due to repetitive or chronic traumatic events. It is distinct from PTSD, which results from a singular traumatic incident.
Individuals suffering from complex PTSD often experience various symptoms such as recurring flashbacks, nightmares, emotional numbness, difficulties in managing emotions, and alterations in self-perception. Trust issues and challenges in forming healthy relationships may also be present.
Complex PTSD primarily stems from prolonged and repetitive traumatic events, like childhood abuse, domestic violence, or exposure to war. Factors that increase the risk of developing complex PTSD include experiencing trauma at an early age, lacking social support, and having prior trauma experiences.
It is essential to highlight that not everyone who undergoes trauma will develop complex PTSD. However, seeking professional assistance is vital for those who do. Trauma-focused therapy has proven to be effective in addressing the symptoms associated with complex PTSD.
To ensure thorough care, integrated treatment programs are crucial. These programs address both complex PTSD and co-occurring disorders, such as substance use disorders, by targeting the root trauma while simultaneously providing support and treatment for related issues.
Causes and Risk Factors for Complex PTSD
Complex PTSD can develop as a result of various causes and risk factors. Traumatic experiences, early life adversity, a lack of social support, pre-existing mental health conditions, and certain biological factors can all contribute to the development of this disorder.
Traumatic experiences, such as childhood abuse, domestic violence, or military combat, can lead to the development of Complex PTSD.
Adverse experiences during childhood, including neglect, emotional or physical abuse, or living in a chaotic environment, are also contributing factors to Complex PTSD.
A weak support system increases the risk of developing Complex PTSD, while a strong support system can help individuals cope with trauma and reduce the likelihood of developing the disorder.
Individuals with pre-existing mental health conditions, such as anxiety or depression, may be more susceptible to Complex PTSD.
Genetic and neurological factors may play a role in the development of Complex PTSD, according to some research.
Let’s consider the story of Sarah as an example to understand the causes and risk factors for Complex PTSD. Sarah experienced emotional and physical abuse throughout her childhood, which had a lasting impact on her mental health, leading to the development of Complex PTSD. Additionally, Sarah lacked a supportive social network, which exacerbated her symptoms. By understanding the causes and risk factors for Complex PTSD, individuals like Sarah can receive the necessary support and treatment for their healing and recovery.

Understanding Alcohol Use Disorder
Alcohol Use Disorder (AUD) is a chronic condition where individuals cannot control or stop drinking alcohol despite negative consequences. Understanding alcohol use disorder is vital in addressing its challenges. It affects millions of people worldwide and has severe physical, psychological, and social effects.
To understand AUD, consider the following points:
1. Prevalence: AUD is common, with around 15 million adults in the United States alone affected. This is a significant public health concern.
2. Risk Factors: Various factors contribute to AUD, including genetics, environment, early alcohol exposure, and mental health conditions like depression or anxiety.
3. Symptoms: People with AUD may have an uncontrollable desire to drink, tolerance to alcohol, withdrawal symptoms when trying to quit, and neglect personal and professional responsibilities due to drinking.
4. Health Consequences: AUD can harm physical and mental health, increasing the risk of liver disease, cardiovascular problems, mental disorders, and even death. It can also strain relationships, cause financial issues, and legal trouble.
5. Treatment Options: Evidence-based treatments for AUD include individual and group therapy, medications, and support groups like Alcoholics Anonymous. Treatment plans should be customized to the individual’s needs and may include a combination of approaches.
6. Supportive Environment: Creating a supportive environment is crucial for individuals recovering from AUD. Involving family and friends, avoiding triggers, and accessing resources like counselors or support groups can greatly enhance the recovery process.
Recognizing the prevalence, risk factors, symptoms, health consequences, available treatments, and the significance of a supportive environment are key in combating this disorder and promoting overall well-being.
What is Alcohol Use Disorder?
Alcohol Use Disorder (AUD) is a chronic condition that involves the inability to control or stop drinking despite negative consequences. It is a severe form of alcohol abuse that can have harmful effects on various aspects of a person’s life.
AUD is diagnosed when individuals experience symptoms such as a strong urge to drink, difficulties in controlling alcohol consumption, withdrawal symptoms when not drinking, and continued alcohol use despite physical or psychological health problems. It is important to note that AUD can affect people of all ages, genders, and backgrounds.
The causes of AUD can be complex and may involve genetic, environmental, and psychological factors. Risk factors for developing AUD can include a family history of alcoholism, early initiation of alcohol use, history of trauma or abuse, and mental health disorders such as depression or anxiety.
Seeking professional help is essential for addressing AUD. Treatment options may include therapy, counseling, support groups, and medication if needed. Having a supportive environment and a strong network of individuals who can provide encouragement during the recovery process is crucial.
If you or someone you know is struggling with AUD, reach out to a healthcare professional or a local support group for assistance. Remember, help is available, and with the right support and treatment, recovery is possible.
Facts: Genetics increase the risk of developing AUD by 40-60%, suggests a study on genetics and alcoholism by experts at Indiana University School of Medicine.
Causes and Risk Factors for AUD
Causes and Risk Factors for AUD are significant in understanding Alcohol Use Disorder (AUD). Excessive alcohol consumption and exposure to specific risk factors contribute to AUD development.
Genetic predisposition is a cause of AUD. Research suggests certain individuals have a higher risk due to genetic factors affecting alcohol metabolism and vulnerability to dependence. Studies show those with a family history of AUD are more likely to develop the disorder.
Environmental factors also play a role. Peer influence, social acceptance of heavy drinking, and exposure to stress increase the risk. Early initiation of alcohol use, like underage drinking, is associated with a higher likelihood of AUD development later.
Individual psychological factors contribute too. Conditions such as depression, anxiety, and PTSD often coexist with AUD. Alcohol may be used as a coping mechanism, leading to AUD development.
It’s important to note that not everyone exposed will develop AUD. The interaction between genetic, environmental, and psychological factors is complex and varies. Understanding these causes and risk factors aids in prevention and treatment by addressing underlying factors.

The Co-occurrence of Complex PTSD and Alcohol Use Disorder
The co-occurrence of Complex PTSD and Alcohol Use Disorder sheds light on the complex challenges individuals face when dealing with these two conditions. This section explores the prevalence of co-occurring disorders and delves into the profound impact they can have on mental health. Uncovering the intertwining nature of Complex PTSD and AUD is essential for understanding the scope of the issue and developing effective strategies for treatment and support. Let’s dive into this intricate dynamic and discover the complexities at play.
Prevalence of Co-occurring Complex PTSD and AUD
The prevalence of co-occurring Complex PTSD and Alcohol Use Disorder (AUD) is a significant issue in mental health. Research shows that a high percentage of individuals experience both disorders simultaneously.
Studies indicate that about half of individuals with Complex PTSD also meet criteria for AUD. “Several psychiatric disorders commonly co-occur with PTSD. Almost half (46.4%) of those with PTSD also meet the criteria for Alcohol Use Disorder (AUD) or a Non-Alcohol Substance Use Disorder,” according to a recent research. (Predictors of alcohol and substance use among people with post-traumatic stress disorder (PTSD): findings from the NESARC-III study, Dell’Aquila, Berle, 2023)
This highlights the strong co-occurrence and suggests a complex relationship between trauma and alcohol misuse. The prevalence of co-occurring Complex PTSD and AUD is higher compared to the rates of either disorder alone. This suggests that individuals with Complex PTSD may be at a higher risk for developing AUD and vice versa. It’s important to note that the exact prevalence may vary depending on the population studied and the diagnostic criteria used.
The co-occurrence of these disorders significantly impacts mental health. Individuals with both Complex PTSD and AUD often experience more severe symptoms, including higher levels of anxiety and depression. They may also have greater difficulty functioning in daily life and are at an increased risk for self-harm and suicide.
Addressing the challenges of co-occurring Complex PTSD and AUD requires integrated treatment approaches that target both disorders simultaneously. This can involve trauma-focused therapies, such as Eye Movement Desensitization and Reprocessing (EMDR), along with substance abuse treatment programs that address alcohol dependence.
Impact of Co-occurring Disorders on Mental Health
Co-occurring disorders, such as complex PTSD and alcohol use disorder (AUD), have a profound impact on mental health. Individuals with co-occurring disorders often experience more severe symptoms and worse treatment outcomes compared to those with a single disorder. The presence of both complex PTSD and AUD can exacerbate anxiety, depression, and difficulties in emotional regulation.
Additionally, co-occurring disorders increase the risk of self-harm, suicide, and accidents related to substance abuse. The combination of trauma-related symptoms and alcohol misuse can impair judgment and lead to risky behaviors.
Furthermore, mental health conditions and substance use disorders can perpetuate one another, resulting in a cycle of negative consequences. While alcohol use may temporarily alleviate distressing PTSD symptoms, it ultimately worsens long-term mental health outcomes.
The impact of co-occurring disorders extends beyond the individual to their relationships, work, and overall quality of life. Individuals with complex PTSD and AUD commonly struggle to manage symptoms, maintain employment, and establish healthy relationships.
Integrating treatment approaches that address both complex PTSD and AUD simultaneously is crucial for improving mental health outcomes. Treating one disorder without considering the other often leads to incomplete recovery and an elevated risk of relapse.
Research has shown that individuals with co-occurring complex PTSD and AUD experience higher rates of hospitalization, suicide attempts, and chronic health conditions compared to those with either disorder alone. Effective treatment strategies that address both disorders can significantly enhance individuals’ well-being and overall quality of life.

Challenges and Issues in Addressing Co-occurring Complex PTSD and AUD
Addressing the challenges of co-occurring complex PTSD and AUD is no easy task. In this section, we’ll uncover the barriers that individuals face when seeking treatment, as well as unique considerations that come into play. Prepare to dive into the importance of integrated treatment approaches, where we’ll explore how combining various therapeutic modalities can offer a glimmer of hope in overcoming these intertwined disorders. It’s time to shed light on the complexities and pave the way towards effective solutions.
Barriers to Treatment
Barriers to Treatment hinder recovery for individuals with co-occurring Complex PTSD and Alcohol Use Disorder (AUD).
Stigma surrounding mental health and addiction prevents seeking help.
Lack of awareness leads to misdiagnosis or inadequate treatment.
Limited specialized care creates accessibility issues.
Financial constraints deter access to treatment.
Dual diagnosis challenges result in fragmented care.
Lack of social support hinders progress.
Addressing these barriers requires a multi-faceted approach.
It includes destigmatization efforts, increased awareness campaigns, improved access to affordable care, integrated treatment programs, and cultivation of supportive environments.
Overcoming these barriers ensures individuals with co-occurring Complex PTSD and AUD receive comprehensive and effective treatment.
Historically, co-occurring mental health and substance use disorders faced significant barriers.
Mental health was stigmatized, leading to inadequate treatment.
Similarly, addiction was seen as a moral failing.
Advancements in research and increased awareness have led to integrated treatment approaches for co-occurring disorders.
Despite progress, barriers remain.
Stigma, limited access to specialized care, and financial constraints complicate treatment.
Efforts are underway to address these barriers.
Promoting awareness, reducing stigma, expanding access to care, and integrating mental health and addiction treatment services create a more supportive environment.
It is essential that individuals with co-occurring disorders receive necessary treatment and support.
Addressing barriers enhances successful outcomes and improves overall well-being.
Unique Treatment Considerations
When treating individuals with co-occurring Complex PTSD and Alcohol Use Disorder (AUD), it is important to consider unique treatment considerations. This involves addressing both trauma-related symptoms of Complex PTSD and addiction-related symptoms of AUD in a comprehensive manner.
1. Integrated Treatment:
An integrated treatment approach is crucial for individuals with co-occurring Complex PTSD and AUD. This approach combines trauma-focused therapy and substance abuse treatment to address both disorders concurrently. By incorporating both mental health and addiction treatment, individuals can receive the comprehensive care needed to address the interconnected nature of these disorders.
2. Trauma-Informed Care:
Treatment providers should employ trauma-informed care when working with individuals with co-occurring Complex PTSD and AUD. This approach recognizes the impact of trauma on an individual’s life and ensures that treatment is sensitive to their needs, promotes safety, and avoids retraumatization.
3. Dual Diagnosis Expertise:
Treatment providers should have expertise in treating dual diagnosis, which refers to the co-occurrence of mental health and substance use disorders. They should possess a deep understanding of both trauma-related symptoms and addiction-related issues to provide effective and tailored treatment.
Importance of Integrated Treatment Approaches
The importance of integrated treatment approaches for individuals with co-occurring Complex PTSD and Alcohol Use Disorder cannot be overstated. Integrated treatment approaches for PTSD and alcohol abuse should address both mental health and substance abuse simultaneously. This comprehensive approach recognizes the intertwined nature of these disorders and ensures unified and coordinated care.
1. Holistic Approach: Integrated treatment approaches recognize the intertwined nature of Complex PTSD and Alcohol Use Disorder. Treating both simultaneously allows for a holistic understanding of the individual’s needs and the development of a comprehensive treatment plan.
2. Coordinated Care: Integrated treatment approaches provide coordinated care from a team of professionals specializing in mental health and substance abuse. This ensures effective treatment of all aspects of the conditions.
3. Dual Diagnosis Treatment: Integrated treatment approaches often include dual diagnosis treatment, which addresses both disorders simultaneously. This approach helps identify underlying causes and triggers for both Complex PTSD and Alcohol Use Disorder.
4. Enhanced Recovery Outcomes: Research shows that integrated treatment approaches yield better and more sustainable recovery outcomes for individuals with co-occurring disorders. By addressing the interconnected issues, individuals have a higher chance of achieving long-term recovery.
5. Supportive Environment: Integrated treatment approaches offer a supportive environment where individuals can share experiences, receive education, and develop coping strategies. This environment is crucial for individuals to feel heard and supported during their recovery journey.
By implementing integrated treatment approaches, individuals with co-occurring Complex PTSD and Alcohol Use Disorder can receive comprehensive and effective care that addresses all aspects of their conditions. This approach recognizes the unique challenges they face and offers a path towards lasting recovery and improved well-being.
Evidence-Based Treatment for Co-occurring Complex PTSD and AUD
Addressing the challenges of co-occurring disorders like Complex PTSD and Alcohol Use Disorder (AUD) requires an evidence-based treatment approach. In this section, we’ll explore the effectiveness of various treatment methods, such as trauma-focused therapy, substance abuse treatment, and integrated treatment programs. Through these approaches, we aim to provide insights and strategies to support individuals facing the complex interplay between trauma and alcohol addiction, paving the way for holistic healing and recovery.
Trauma-Focused Therapy
Trauma-Focused Therapy is crucial in treating individuals with co-occurring Complex PTSD and Alcohol Use Disorder (AUD). It focuses on addressing traumatic experiences that contribute to both disorders.
1. The therapy aims to help individuals process and make sense of their trauma. Techniques like cognitive restructuring, Eye Movement Desensitization and Reprocessing (EMDR) sessions for PTSD, and exposure therapy are used to actively address and explore underlying trauma.
2. This therapy approach prioritizes creating a safe and supportive environment. Therapists work collaboratively with clients to establish trust and provide a secure space to discuss and process traumatic memories.
3. Trauma-Focused Therapy teaches coping skills and techniques to manage distressing symptoms resulting from trauma. These skills include relaxation techniques, grounding exercises, and emotion regulation strategies.
4. Additionally, this therapy approach recognizes the impact of trauma on relationships and daily functioning. It aims to improve social and interpersonal skills, helping individuals cultivate healthier relationships and enhance their overall quality of life.
5. Research demonstrates that trauma-focused therapy significantly reduces symptoms of Complex PTSD and AUD. By addressing the underlying trauma, successful recovery becomes more likely.
Incorporating trauma-focused therapy into treatment plans increases the chance of overcoming challenges and achieving lasting recovery for those with co-occurring Complex PTSD and AUD. It is an evidence-based approach that provides hope and healing for these two disorders.
Substance Abuse Treatment
Substance abuse treatment plays a crucial role in effectively addressing co-occurring complex PTSD and alcohol use disorder (AUD). The provision of appropriate interventions not only promotes recovery but also improves mental health outcomes.
In substance abuse treatment, evidence-based approaches are employed to target the specific needs of individuals with co-occurring disorders. These approaches encompass various methods:
1. Behavioral therapies: Behavioral therapies, including cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT), are highly effective in treating substance abuse. They assist individuals in recognizing and modifying harmful thoughts, emotions, and behaviors related to substance abuse.
2. Medications: Alongside behavioral therapies, medications can be used to manage withdrawal symptoms and cravings associated with substance abuse. Commonly prescribed medications for alcohol addiction include Naltrexone and Acamprosate.
3. Support groups: Support groups such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) provide a nurturing environment for individuals who have had similar experiences. These groups offer guidance and encouragement throughout the recovery process.
4. Integrated treatment programs: Integrated treatment programs tackle complex PTSD and AUD concurrently. These programs incorporate therapies for both disorders, resulting in a comprehensive treatment plan. By addressing co-occurring disorders simultaneously, individuals have a higher chance of better outcomes and reducing the risk of relapse.
It is crucial to tailor substance abuse treatment to an individual’s specific needs and circumstances. A personalized approach ensures the most effective treatment to address unique challenges and enhance overall well-being.
Integrated Treatment Programs
Integrated Treatment Programs offer comprehensive care for individuals with co-occurring complex PTSD and Alcohol Use Disorder (AUD). These programs recognize the connection between mental health and substance abuse and address both disorders simultaneously.
-
Collaborative Approach: Integrated Treatment Programs involve a team of professionals, including therapists, psychiatrists, and addiction specialists, who collaborate to develop an individualized treatment plan. This collaborative approach ensures that both disorders are effectively addressed.
-
Dual Diagnosis Treatment: Integrated programs provide tailored therapies specifically for individuals with co-occurring disorders. These therapies, such as trauma-focused therapy, Cognitive-Behavioral Therapy (CBT), and Dialectical Behavior Therapy (DBT), aim to address the symptoms of complex PTSD and the underlying causes of alcohol use.
-
Medication Management: In some cases, medication may be prescribed to manage the symptoms of complex PTSD and support recovery from AUD. This may include antidepressants, anti-anxiety medications, or medications to reduce cravings and withdrawal symptoms.
-
Education and Skill-Building: Integrated Treatment Programs focus on equipping individuals with practical tools and coping strategies to manage their mental health and substance use. This includes stress management techniques, relapse prevention skills, and healthy lifestyle practices.
-
Long-Term Support: After completing an integrated treatment program, ongoing support is crucial for maintaining recovery. This may involve therapy, support groups at an outpatient drug rehab, and assistance in accessing community resources to promote sustained well-being.
Sarah, a 32-year-old woman, sought help for her co-occurring complex PTSD and AUD. She enrolled in an Integrated Treatment Program that offered individual and group therapy, addressing both her trauma history and alcohol dependence. Through trauma-focused therapy and substance abuse treatment, Sarah gained a deeper understanding of the connections between her PTSD symptoms and alcohol use. Integrated Treatment Programs provided her with the tools to effectively manage her symptoms and develop healthier coping mechanisms. With ongoing support and relapse prevention techniques, Sarah has been able to maintain her sobriety and improve her overall well-being.

Recovery and Support for Individuals with Co-occurring Complex PTSD and AUD
Recovery from co-occurring complex PTSD and alcohol use disorder (AUD) is a journey that requires a strong support system, effective coping strategies, and relapse prevention techniques. In this section, we will explore how building a strong support system, practicing self-care, and implementing coping strategies can aid individuals in their path to recovery. Additionally, we will delve into the importance of utilizing relapse prevention techniques to maintain long-term sobriety and mental wellness. Let’s uncover the key elements that facilitate healing and growth in the face of these challenging co-occurring disorders.
Building a Strong Support System
Building a strong support system is vital when it comes to individuals with co-occurring complex PTSD and alcohol use disorder (AUD). It plays a crucial role in promoting recovery and providing essential assistance. Here are some important factors to consider when establishing a strong support system:
1. Surround yourself with trustworthy individuals: It is crucial to be surrounded by understanding, non-judgmental, and supportive people. Trust forms the foundation of a strong support system.
2. Join support groups: Engaging in Alcoholics Anonymous or PTSD support groups allows you to connect with others who have had similar experiences and fosters a sense of belonging.
3. Seek professional help: Therapists, counselors, and addiction specialists can offer guidance, tools, and techniques to help you cope with complex PTSD and AUD. Their expertise enhances the recovery process.
4. Involve family and close friends: Engaging supportive family members and close friends in your journey to recovery provides a solid foundation of love and understanding.
5. Develop a relapse prevention plan: It is crucial to create a plan with your support system that includes coping strategies, emergency contacts, and activities to distract yourself from cravings or triggers.
6. Maintain regular communication: Keeping your support system updated on your progress, struggles, and victories through open communication ensures that everyone can offer the necessary support.
7. Emphasize accountability: Your support system can play a pivotal role in helping you stay accountable for your actions and decisions. They can remind you of your goals and steer you away from harmful behaviors.
Remember, building a strong support system is an ongoing process that requires effort and engagement from everyone involved. With a solid support system, individuals with co-occurring complex PTSD and AUD can find strength, encouragement, and invaluable assistance on their path to recovery.
Self-Care and Coping Strategies
When dealing with co-occurring Complex PTSD and Alcohol Use Disorder (AUD), self-care and coping strategies are crucial for maintaining well-being and managing symptoms. Here are some strategies that can benefit individuals facing these disorders:
– Incorporate self-care and coping strategies, such as practicing mindfulness and relaxation techniques like deep breathing exercises, meditation, and yoga, to naturally reduce stress and promote emotional stability.
– Engage in regular physical exercise as part of your self-care routine. This can improve mood, reduce anxiety and depression, and promote overall well-being.
– Prioritize getting enough quality sleep and establish a consistent sleep routine. This is especially important since sleep disturbances are common in both Complex PTSD and AUD.
– Seek support from a therapist or support group. Talking to someone who understands and can help you process trauma and gain tools for managing symptoms is an essential part of self-care.
– Find healthy coping mechanisms that do not involve alcohol or substance use. Consider activities like journaling, art therapy, listening to music, or engaging in hobbies.
It’s important to remember that self-care and coping strategies may vary between individuals. Personalizing your practices based on your individual needs and preferences is essential.
Today, individuals with co-occurring Complex PTSD and AUD can access support, evidence-based treatments, and resources to enhance their well-being and facilitate their journey towards recovery. By incorporating self-care and coping strategies into their daily lives, individuals can effectively manage their symptoms, improve their overall quality of life, and create a foundation for lasting recovery.
Relapse Prevention Techniques
Relapse prevention techniques are vital for individuals with co-occurring Complex PTSD and Alcohol Use Disorder (AUD) in order to maintain recovery and avoid harmful substance use. Effective strategies include:
1. Identify triggers and high-risk situations: Recognize people, places, and emotions that may contribute to cravings or temptations to drink. Develop strategies to avoid or manage them.
2. Develop coping skills: Learn healthy and effective coping mechanisms, such as stress management techniques, engaging in fulfilling activities, and seeking support from a therapist or support group.
3. Create a relapse prevention plan: A roadmap for maintaining sobriety, including steps to take if cravings arise and a list of supportive individuals to reach out to.
4. Build a strong support system: Have a supportive network of family, friends, or individuals in recovery for encouragement and accountability. Regularly attend support group meetings or therapy sessions.
5. Practice self-care: Take care of oneself physically, emotionally, and mentally. This includes getting adequate sleep, eating a nutritious diet, regular exercise, and practicing self-compassion.
6. Seek professional help: If cravings become overwhelming or there is a risk of relapse, it is essential to seek professional help. Therapists and addiction specialists can provide guidance and evidence-based interventions.
Frequently Asked Questions
What is the relationship between PTSD and substance use disorder (SUD)?
There is a strong link between trauma exposure and SUD, with studies showing that individuals who have experienced physical or sexual abuse are more likely to report substance misuse. Substance use can be seen as self-medication for PTSD symptoms, as individuals try to numb out distress or avoid confronting trauma.
What is complex PTSD and how is it different from PTSD?
Complex PTSD, recognized as a distinct condition by the World Health Organization, involves exposure to prolonged or repetitive traumatic events and severe problems in affect regulation and sustaining relationships. Unlike PTSD, which is primarily associated with single traumatic events, complex PTSD is characterized by ongoing trauma and difficulties in emotional regulation.
What are some evidence-based treatments for co-occurring PTSD and SUD?
Trauma-focused cognitive behavioral psychotherapies like Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT) have shown to be beneficial for individuals with PTSD and SUD. These treatments target both the trauma symptoms and substance use behaviors. Combining medication and psychotherapy, such as PE with naltrexone, can also be more effective in reducing substance use.
How can clinicians assess and treat co-occurring PTSD and SUD in veterans?
Clinicians should assess potential underlying trauma symptoms using tools like the Trauma History Questionnaire and the PTSD Checklist when treating veterans with SUD. Trauma-focused treatments like PE and CPT should be offered to veterans with co-occurring PTSD and SUD based on VA policy. Ongoing assessment and measurement based care are critical for understanding the needs and progress of veterans in treatment.
What are the challenges in treating co-occurring PTSD and SUD?
Individuals with co-occurring PTSD and SUD tend to have poorer treatment outcomes compared to those without such comorbidity. Non-exposure-based psychosocial treatments have shown limited benefit, and medication trials with selective serotonin reuptake inhibitors have had limited success. There is a need for further research on the best approaches to treat co-occurring PTSD and SUD.
What are the policy and practice recommendations for addressing co-occurring PTSD and SUD?
The 2017 VA/DoD Clinical Practice Guideline recommends evidence-based treatments for PTSD and SUD be available to veterans. VA requires that all Medical Centers provide access to trauma-focused treatments like Prolonged Exposure (PE) or Cognitive Processing Therapy (CPT) for veterans with PTSD. Shared decision making using a patient-centered approach and measurement based care should be used to engage and retain veterans in care.