Key Takeaway:
- Co-occurring disorders, or the coexistence of mental health and substance use disorders, is common in addiction treatment. Understanding the relationship between mental health and addiction is key to providing effective treatment.
- An integrative approach that addresses both mental health and substance use disorders is essential for sustainable recovery. This approach may include cognitive behavioral therapy, medication-assisted treatment, and other evidence-based therapies.
- Prevention and early intervention can stop the cycle of addiction before it progresses. Screening and assessment for co-occurring disorders, education and awareness about mental health and substance use, and addressing disparities in healthcare are important steps in preventing and treating co-occurring disorders in addiction.
Do you struggle with a mental health disorder and addiction? You’re not alone. This article focuses on how to address co-occurring disorders to ensure successful addiction treatment.
Understanding Co-occurring Disorders
It s no secret that addiction is a complex disease that affects individuals from all walks of life. But what many people don t know is that addiction rarely occurs in isolation. More often than not, addiction occurs alongside one or more mental health disorders, collectively known as co-occurring disorders.
In this section, we ll take a deep dive into understanding co-occurring disorders and their impact on addiction treatment. We ll start by defining what co-occurring disorders are and how they relate to addiction. Then, we ll talk about the most common co-occurring disorders and how they affect addiction treatment. Finally, we ll explore the risk factors associated with co-occurring disorders and why they often occur together. Get ready to gain a comprehensive understanding of the relationship between mental health and addiction.

Defining Co-occurring Disorders: Understanding Mental Health and Addiction
Understanding the relationship between mental health and addiction is crucial in defining co-occurring disorders. When an individual experiences both a mental disorder and substance use disorder at the same time, it is referred to as co-occurring or comorbid disorders. This condition requires comprehensive and integrated treatment to address both mental health disorders and addiction effectively.
Comorbidity of mental illnesses and substance abuse is not merely coincidental; there are numerous reasons why they occur together. Certain psychological factors can lead to a person self-medicating their symptoms with drugs or alcohol, while continued drug abuse could damage the brain s reward system and eventually alter normal cognitive functioning resulting in a predisposition for a broader array of mental illnesses. Therefore, identifying the underlying causes of an individual’s drug use and any accompanying symptoms will help families, healthcare professionals, and loved ones better understand co-occurring disorders.
Co-occurring disorders affect people from all walks of life – age groups, ethnicities, races, cultures, sexual orientations. The absence of effective diagnosis accounting for both physical issues can complicate measurements regarding concurrent conditions in research studies. This may result in their underreporting as statistic inadequacy reflects underrepresentation regarding occurrences around mental health stigmas. It highlights how imperative an unbiased acknowledgement of different identities affected by co-occurring diagnoses is essential.
If you’re worried about someone who might be struggling with co-occurring disorders that blur the lines between addiction-treatment goals and aesthetic restoration- seek professional medical advice immediately. Shed light on your difficulties openly; books suggest seeking support from family members who ought to facilitate comfort over trauma alongside pre meditated solutions like cognitive behavior therapy (CBT), mutual aid groups such as Narcotics Anonymous meetings or similar twelve-step organizations regularly partaking essential step work through guided collaboration.
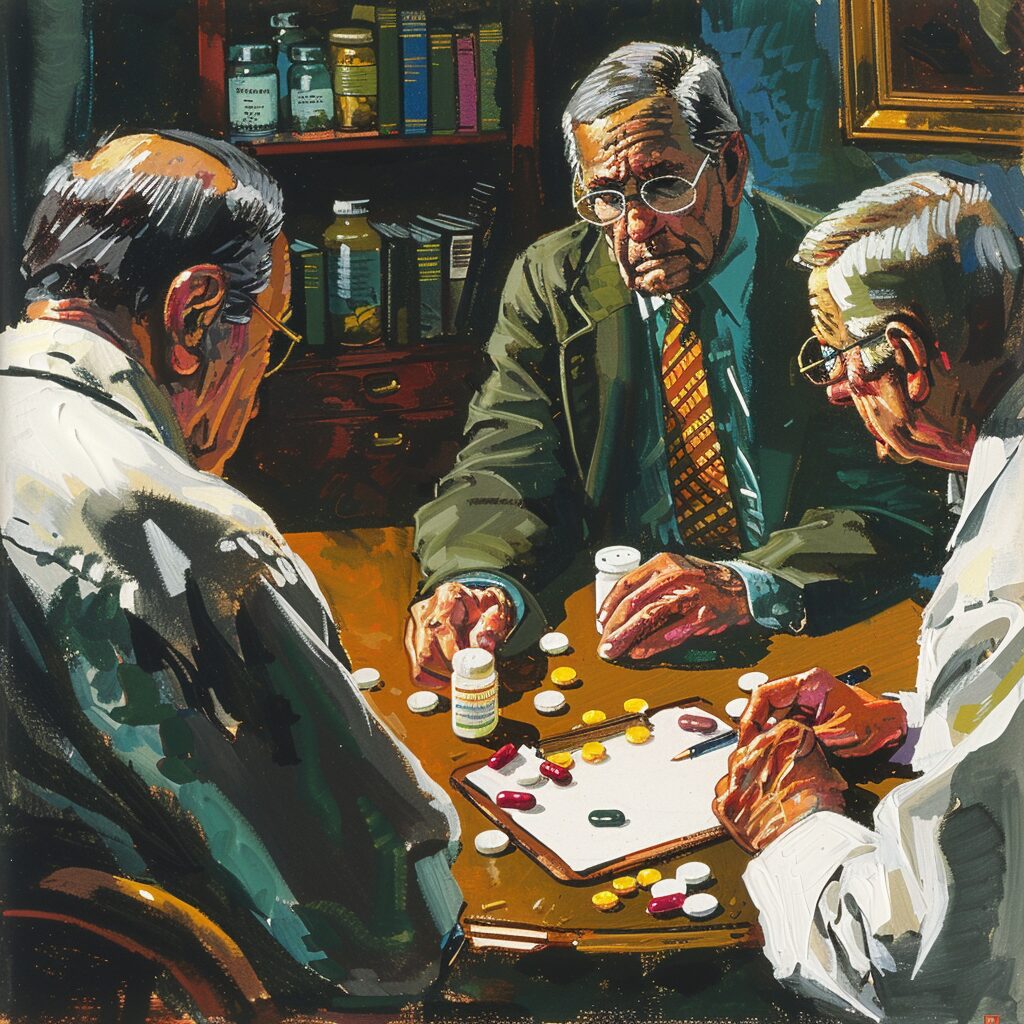
The existence of multiple conditions that lead to complex management demands addressing common comorbidity factors while designing an intensive care plan tailored to specific patient needs. Approaches including medications, counseling and support treatment programs, identifying co-occurring disorders at the outset of an addiction treatment program leads to the best possible outcome for recovery enhancing not just their substance free future but overall mental health & physical wellbeing.
Co-occurring Disorders in Addiction Treatment: Understanding the Common Comorbidities
Addiction is a complex issue that requires comprehensive treatment. Co-occurring disorders in addiction treatment means addressing multiple conditions simultaneously. It is common for many individuals with substance use disorders to have other mental health issues, such as anxiety, depression, personality disorders, or even post-traumatic stress disorder (PTSD). In fact, studies show that the prevalence of co-occurring disorders in addiction treatment can be as high as 50%.
The relationship between addiction and co-occurring disorders is complex. Often a person turns to drugs or alcohol to cope with an underlying mental health condition or trauma – which over time becomes an addiction. On the other hand, long-term substance abuse changes the chemistry of the brain and often exacerbates underlying psychiatric conditions. Therefore, treating only one condition is not enough to achieve successful recovery.
Co-occurring Disorders in Addiction Treatment: Understanding the Common Comorbidities provides valuable information on how to approach these intertwined problems systematically. It addresses ways to diagnose and treat dual diagnosis clients and empowers medical professionals with essential skillsets required for adequate patient care.
Pro Tip: Patients who struggle with co-occurring disorders require individualized treatment plans that accurately address each condition present in order to better manage their overall care.
With so many factors at play that lead to co-occurring disorders in addiction treatment, it’s important to understand both the individual risk factors and why they often occur together. Identifying the Risk Factors for Co-occurring Disorders: Why They Often Occur Together will delve deeper into this issue – keep reading!
Identifying the Risk Factors for Co-occurring Disorders: Why They Often Occur Together
Identifying the risk factors for co-occurring disorders is crucial as these often occur together. People struggling with addiction frequently experience other mental health issues. This connection between substance use and mental health makes it essential to understand why these disorders often occur simultaneously.
Co-occurring disorders are best explained by understanding the concept of self-medication. People struggling with mental health issues may use drugs or alcohol to alleviate their symptoms. For example, someone experiencing anxiety may drink alcohol to calm down. This can lead to developing an addiction in the long run.
There are several reasons why co-occurring disorders often occur together. Genetics and environmental factors play a vital role in this phenomenon. Family history of substance abuse, exposure to trauma, and other life stressors can increase one’s susceptibility to both addiction and mental illness.
Recent studies have identified several risk factors that contribute to co-occurring disorders. These include childhood trauma, chronic stress, social isolation, lack of motivation, and low self-esteem. Identifying these specific risk factors can help healthcare professionals provide more effective treatment for patients.
If you or someone you know is dealing with a co-occurring disorder, seek professional help immediately. Treatment options such as cognitive-behavioral therapy (CBT) and medication-assisted therapy (MAT) have shown promising results in treating addiction alongside underlying mental health conditions. Additionally, implementing lifestyle changes such as regular exercise, healthy eating habits, and sufficient sleep can improve both physical and emotional well-being.
Navigating a co-occurring disorder can be challenging but not impossible to overcome with proper care and management strategies in place. In the section below, we’ll explore different treatment options available for people battling dual diagnosis; stay tuned!
Treatment for Co-occurring Disorders in Addiction
As someone who has been in addiction treatment, I understand how important it is to address not only substance use disorders but also any underlying mental health conditions. In this part, our focus will be on exploring the different treatment options that exist for co-occurring disorders in addiction. We will be discussing why it is essential to take an integrative approach that treats both the mental health condition and the substance use disorder simultaneously.
We will also explore the benefits of Cognitive Behavioral Therapy, which can address both mental health and substance use disorders. Finally, we will delve into the role of medication-assisted treatment in balancing the brain chemistry for sustainable sobriety.

Integrative Approach: Why Treating Both is Essential
Integrative Approach: Why Treating Both is Essential
When it comes to treating addiction, many people might assume that the solution would be to simply focus on ending the substance use. However, this approach can often fall short, especially when there are co-occurring disorders present such as mental health issues. That’s why an integrative approach – one that addresses both addiction and any underlying mental health concerns – is absolutely essential.
An integrative approach involves comprehensive treatment that targets not just the external behaviors associated with addiction, but also the internal factors contributing to it. This includes examining and addressing any underlying mental health diagnoses or other psychological issues like trauma or anxiety. By treating the root causes of addiction alongside the addictive behavior itself, an integrative approach can help clients regain control over their lives in a more sustainable way.
The importance of treating both addiction and co-occurring disorders cannot be overstated. In fact, research has shown that individuals struggling with both conditions tend to have poorer outcomes overall without integrated treatment. By taking a holistic approach to treatment, we’re able to address all aspects of a client’s life and provide them with the tools they need for lasting recovery.
As someone who has struggled with addiction and co-occurring disorders myself, I know firsthand how important this type of treatment can be. For years, I tried unsuccessfully to get sober without addressing my underlying mental health struggles. It wasn’t until I found a program that provided integrated care that I was finally able to make real progress towards recovery.
Up next: Cognitive Behavioral Therapy: Addressing both Mental Health and Substance Use Disorders in a Way That Works
Cognitive Behavioral Therapy: Addressing both Mental Health and Substance Use Disorders
Addressing both mental health and substance use disorders, Cognitive Behavioral Therapy (CBT) has proven to be an effective treatment option for individuals suffering from co-occurring disorders. CBT is a form of psychotherapy that focuses on changing negative thought patterns and behaviors that contribute to mental health issues and substance abuse. This type of therapy helps individuals develop coping skills and self-regulation techniques that can be used in everyday life.
CBT works by teaching individuals how to identify triggers for their substance use or mental health symptoms. By understanding these triggers, individuals can learn new ways of responding to them, rather than turning to substances or negative thought patterns. This type of therapy is time-limited, providing short-term interventions that help individuals learn new skills quickly.
One valuable aspect of CBT for co-occurring disorders is that it can address both the substance use disorder and the underlying mental health issues simultaneously. By doing so, this type of therapy helps individuals achieve greater long-term success in maintaining sobriety and improving overall mental health.
Interestingly, CBT has also proven effective in treating a wide range of other mental health issues, including anxiety disorders, depressive disorders, eating disorders, personality disorders, and more.
Studies have shown that around 50% of people with substance abuse problems also have at least one co-occurring mental illness (Substance Abuse and Mental Health Services Administration). Therefore, treatments like CBT are crucial in addressing both the addiction and the underlying condition. If you are looking for more information on addressing trauma in addiction treatment, click here.
As I delve into the next section on Medication-Assisted Treatment: Balancing the Brain Chemistry for Sustainable Sobriety, I am intrigued by the potential overlap between medication-assisted treatment options and cognitive-behavioral therapies.
Medication-Assisted Treatment: Balancing the Brain Chemistry for Sustainable Sobriety
The path to sobriety is often a difficult one, especially when it comes to the treatment of individuals with co-occurring disorders. However, there is hope in using Medication-Assisted Treatment, which can balance the brain chemistry for sustainable sobriety.
Medication-Assisted Treatment (MAT) involves the use of medication to treat addiction by suppressing cravings and withdrawal symptoms. This helps individuals stay focused on recovery and have a greater chance of long-term success. MAT usually includes cognitive behavioral therapy or other behavioral therapies as well.
One reason MAT works so effectively is because it targets the biological aspect of addiction. Substance abuse affects the natural balance of brain chemicals, such as dopamine and serotonin, that keep us feeling motivated and happy. The medications used in MAT work to stabilize this imbalance and reduce cravings.
While some may argue against using medication in addiction treatment, MAT has been proven effective with years of research backing it up. It has been shown to reduce drug use, overdose deaths, criminal activity, and more.
In fact, according to the Substance Abuse and Mental Health Services Administration (SAMHSA), “Research shows that a combination of medication and therapy can successfully treat these disorders, and for some people struggling with addiction, MAT can help sustain recovery.”
With its proven success rates and ability to balance brain chemistry in a sustainable way, Medication-Assisted Treatment is becoming an increasingly popular method for treating those struggling with co-occurring disorders.
And now onto how we can prevent those co-occurring disorders altogether – but that will have to wait until my next section!
Preventing Co-occurring Disorders in Addiction
When it comes to addiction treatment, addressing co-occurring disorders can play a critical role in achieving lasting recovery. In this part of the article, I ll be discussing some key strategies for preventing co-occurring disorders in addiction.
First up, we ll take a look at the power of early intervention and how stopping addiction in its tracks can prevent other mental health conditions from taking hold. We ll then move on to exploring the value of screening and assessment in identifying co-occurring disorders.
Finally, we ll delve into the importance of education and awareness in promoting mental health and substance use awareness for prevention. So stick with me as we explore these vital components of preventing co-occurring disorders in addiction.

Early Intervention: Stopping the Cycle of Addiction Before It Progresses
Early intervention is the key to stopping the harmful and potentially deadly cycle of addiction. By intervening early, we have a chance to help those struggling with addiction before it progresses and causes long-term damage. The approach involves identifying and addressing warning signs in individuals who are at risk of addiction, such as those with a family history or previous traumatic events.
Early intervention works by identifying problematic behavior and providing support and resources to address the underlying issues. This may include counseling, education on coping skills, and access to addiction treatment programs. It’s important to note that early intervention doesn’t just benefit the individual struggling with addiction but can also improve their relationships with family and friends.
Research has shown that early intervention can reduce drug use and related harm, including hospital admissions due to overdose or infection. It’s also been demonstrated that intervening early can lead to better outcomes for children living in households affected by substance abuse.
In one study published in the Journal of Substance Abuse Treatment, researchers found that children exposed to parental substance abuse who received comprehensive services (including parenting skills training, therapy sessions for both parent and child, regular medical check-ups, etc.) during their first five years had significantly lower rates of behavior problems compared to those who did not receive any such interventions.
A personal story from someone who benefitted from early intervention:
“My life was spiraling out of control due to my alcoholism when my friend encouraged me to seek help. I reluctantly agreed and was met with kindness and understanding from a counselor at an addiction treatment center. Through their support and guidance, I was able to get sober and turn my life around. Without their early intervention, I shudder to think where I would be today.”
Feeling overwhelmed by your experience with co-occurring disorders? Don’t worry there are ways you can get started on your path towards recovery without feeling afraid or uncertain about what lies ahead.
Screening and Assessment: Identifying Co-occurring Disorders in Addiction Treatment
Every individual who struggles with addiction requires an intensive level of care, support and treatment. As substance abuse often arises out of underlying mental health issues, it is imperative to identify the co-occurring disorders in addiction treatment that require attention.
Screening and Assessment: Identifying Co-occurring Disorders in Addiction Treatment is a critical component of recovery from addiction. It involves evaluating individuals for any additional mental or psychiatric issues that may be contributing to or exacerbating their addiction. This screening is done through mental health assessments and personalized questionnaires designed to determine the individual’s mental health history, current symptoms, and any other relevant information.
The screening process helps healthcare professionals to determine which type of treatments are most suitable for the patient s unique needs. By identifying co-occurring disorders early on, medical professionals can tailor therapy options more specifically to the person s requirements. Further interventions can then be put into place to address these disorders and help prevent relapse.
When assessing patients for co-occurring disorders in addiction treatment, multiple factors such as age, family history, past experiences with drug use or mental illness are taken into account. Furthermore, some biological markers like personality traits might make certain patients inherently vulnerable to developing mental illnesses. With this knowledge on hand specialists can better compile a prescription for recovery suited particularly to each person’s individual needs.
While screening methods have been widely used for decades now, they have continued evolving due to clinical research that has enabled superior accuracy in making diagnoses at an earlier stage. Now different types of therapies are used in addiction treatment to assist those struggling with alcohol/drug addiction by promoting diagnosis and quickly adapting appropriate interventions. To learn more about the different types of therapies used in addiction treatment, visit this link.
Recovering from substance abuse is challenging enough without dealing with additional undiagnosed co-occurring disorders. So if you haven’t had the screening yet – don t hesitate! Understanding how untreated trauma affects our lives empowers us all as we continue forward working towards benefitting ourselves and society as whole.”
Education and Awareness: Promoting Mental Health and Substance Use Awareness for Prevention
Education and Awareness: Promoting Mental Health and Substance Use Awareness for Prevention is an effective way to address co-occurring disorders in addiction treatment. This approach emphasizes educating people about the interconnection between substance use and mental health issues. It aims to promote awareness about the need for prevention by increasing knowledge about the risk factors of developing a co-occurring disorder.
This method works because it helps individuals understand that there is a strong link between mental illness and substance use disorders. The more people learn about the connection between these two conditions, the better they can recognize risk factors and take appropriate steps towards prevention. In this way, Education and Awareness: Promoting Mental Health and Substance Use Awareness for Prevention can increase the chances that someone will reach out for help before developing a more severe problem.
Moreover, increased awareness around co-occurring disorders helps reduce stigma surrounding mental health issues. When people understand that substance use disorders are often comorbid with mental illness, they may be less likely to judge others who suffer from addiction or label them as “weak” or “irresponsible.” This reduced stigma may lead to more individuals seeking help without fear of judgment.
Pro Tip: If you have concerns about your own substance use habits or those of someone you know, try reaching out for information. Knowledge can be very empowering in terms of taking control over our health outcomes!
Don’t let co-occurring disorders hold you back from living your best life – in fact, addressing them head-on could be key to long-term wellness. So let’s explore some common challenges associated with treating these complex conditions.
Challenges in Treating Co-occurring Disorders in Addiction
As someone who has worked in addiction treatment for several years, I’ve seen firsthand the challenges that come with addressing co-occurring disorders. In this part of the article, we’ll explore some of the major challenges faced in treating co-occurring disorders in addiction. We’ll discuss the issues related to a lack of access to treatment and disparities in healthcare, the stigma and discrimination surrounding mental health disorders, and the limited funding allocated for addressing the growing demand for addiction treatment in the U.S. Through examining these issues, we hope to shed some light on the obstacles that need to be addressed to improve the chances of successful treatment for those experiencing co-occurring disorders.

Lack of Access to Treatment: Addressing Disparities in Healthcare
Access to adequate healthcare is a critical component in improving the health outcomes for individuals. However, not everyone has access to quality healthcare services equally, and this creates disparities in providing effective treatment. ‘Lack of Access to Treatment: Addressing Disparities in Healthcare’ points to this critical gap that exists today.
When it comes to providing effective treatment, access issues play a critical role. Lack of access stems from various factors, including affordability, limited availability of resources, inadequate infrastructure, insurance coverage limitations, social norms and cultural barriers. Such barriers often create issues when delivering treatment options for chronic conditions like addiction or co-occurring disorders.
‘Disparities in healthcare’ signifies the unequal distribution of healthcare among different people or communities based on factors like race/ethnicity, income level, geographic location etc. The disparities lead to inequality in accessing diagnoses or treatments that contribute significantly to poor health outcomes.
It is essential to note that addressing these healthcare disparities requires a collaborative effort between policymakers, government agencies as well as the private sector institutions that work within the broader scope of the healthcare system. It is also crucial to consider demographic characteristics such as age and gender while designing interventions and strategies that seek to address these problems.
According to a report by Kaiser Family Foundation (KFF) published in April 2021 “Black adults are more likely than white adults to report unmet mental health needs,” showcasing one discrepancy amongst dozens such pockets with unequal access.
As I contemplated how we can bridge these access gaps regarding treating co-occurring disorders in addiction treatment effectively one thought came immediately.
Dealing with Stigma and Discrimination: Overcoming the Barriers to Treatment
Dealing with Stigma and Discrimination: Overcoming the Barriers to Treatment is a major challenge that people face when seeking treatment for addiction or co-occurring disorders. Unfortunately, the social stigma attached to addiction can prevent people from seeking help, leading to untreated conditions or even worse outcomes.
Stigma and discrimination surrounding addiction are often based on misinformation and stereotypes about the behavior, character, and motivation of individuals who struggle with substance abuse. People living with addiction injuries may feel embarrassed or ashamed to reach out for help due to their perceptions of societal judgments.
One way of combating drug dependency stigmatization is through education activities aimed at raising awareness about its adverse effects. This increases knowledge about its pathophysiology, evidence-based treatments, and correctional mechanisms. Educational institutions must also develop curricula that encourage open communication on this topic.
Another practical approach is creating supportive systems where support groups come together to collaborate on new ways of assisting those in need. These collaborative efforts include government organizations with non-profit organizations whose central agenda is providing health services to drug addicts for purposes of harm reduction.
To minimize discrimination around mental health disorders like substance abuse, it’s essential first we acknowledge that anybody can be hit by these diseases regardless of age or level of success. People facing challenges within themselves should never feel victimized by society; instead, they need support like any other member.
Next up – Limited Funding: Advocating for Resources to Address the Growing Demand – When resources are scarce in facilities aimed at minimizing drug dependence rate, patients’ number exceeds available resources; how do we bridge it?
Limited Funding: Advocating for Resources to Address the Growing Demand
It’s a common problem in addiction treatment centers that there isn’t enough funding to address the increasing demand for their services. Limited funding makes it challenging for treatment centers to provide adequate care for their patients, especially when dealing with co-occurring disorders.
With limited funding, it’s difficult for these centers to offer the required resources to those who need them. The reasons behind this are many; firstly, most of these centers rely on grants and other government funding, which may be scarce or insufficient. Secondly, with the growing demand for services, some addicts may end up waiting months or even years before getting help.
To address limited funding, advocates have been mobilizing and seeking support from various organizations and policymakers. For example, they have been lobbying the government to increase funding for addiction treatment programs so that treatment centers can provide better care.
Furthermore, advocates are also pushing for more effective insurance coverage of addiction treatment services. Many insurance policies do not adequately cover the cost of addiction treatment, making it hard for people who need these services to access them.
I know firsthand how detrimental limited funding can be because I battled substance abuse myself. When I decided it was time to get help and sought out a rehab center, I was shocked at how few resources there were available. In hindsight, I feel grateful that I was able to overcome my addiction despite limited resources.
Understanding the Importance of Treating Co-occurring Disorders in Addiction
Understanding the importance of treating co-occurring disorders in addiction is crucial for effective recovery. When individuals suffer from both substance abuse and mental health issues, it becomes challenging to treat only one without considering the other. Co-occurring conditions can worsen addiction outcomes, making it imperative to address them together.
Research indicates that up to 60% of people with addiction also have a co-occurring mental illness like depression or anxiety disorder. This statistic alone emphasizes the need to understand and treat both conditions simultaneously. When both issues are neglected, individuals risk a higher chance of relapse even after completing addiction treatment.
Moreover, co-occurring disorders can be challenging due to unique challenges that come with managing multiple symptoms at once. For instance, if someone has anxiety and addiction, anxiety triggers may lead them back to substance abuse even after getting sober from their addiction. Treating mental illness reduces the likelihood of relapse while addressing potential triggers and ensuring long-lasting healing effects.
Furthermore, addressing underlying mental illnesses restores self-esteem and hope so individuals can develop better coping mechanisms during stressful times. In fact, research shows that treating co-occurring conditions leads to improved social functioning, better overall quality of life and reduced legal issues related to drug abuse.
If you or a loved one is struggling with co-occurring disorders, consider seeking professional help for comprehensive treatment approaches like Cognitive Behavioral Therapy (CBT) or Medication-Assisted Treatment (MAT). These techniques are known to treat both conditions simultaneously by targeting underlying psychological problems causing addiction behaviors.
It’s time we devote adequate resources towards understanding how to manage co-occurring disorders effectively. By focusing on this issue more precisely in addiction treatment settings, we increase the chances for successful long-term recovery outcomes for patients dealing with more than one condition.
The Role of Holistic and Comprehensive Treatment in Achieving Lasting Recovery
Achieving lasting recovery is no easy feat, and it requires a comprehensive approach that includes holistic treatment. Holistic and comprehensive treatment is crucial in addressing the root cause of addiction, which for many individuals, also includes co-occurring disorders such as mental health conditions.
The role of holistic and comprehensive treatment lies in providing a well-rounded approach to addiction recovery that tackles not just the physical aspect of addiction but also the emotional, social, and spiritual factors that contribute to substance use disorder. This type of treatment encompasses a range of therapies and interventions, including counseling, group therapy, medication-assisted treatment (MAT), mindfulness-based practices such as yoga and meditation, nutrition education, and exercise.
Holistic and comprehensive treatment works because it addresses the underlying causes of addiction. Many people who struggle with substance use disorder do so because they are trying to cope with an underlying emotional or psychological pain. By providing support through counseling and other therapeutic interventions, individuals can learn how to manage their symptoms without resorting to drugs or alcohol.
Moreover, holistic treatment recognizes that everyone’s path to recovery is unique; there is no one-size-fits-all solution to overcoming addiction. Instead, this approach takes into account the individual’s needs and preferences when developing a personalized plan of care.
One key aspect of holistic and comprehensive treatment is its focus on treating co-occurring disorders that are commonly associated with addiction. Often undiagnosed or inadequately treated mental health conditions can trigger drug or alcohol abuse. By properly diagnosing any co-occurring disorders during intake assessment – like anxiety or depression – healthcare professionals can tailor treatments more effectively.
While the journey towards lasting recovery isn’t an easy one, stories like Ava’s validate why the holistic approach should be adopted universally for successful rehabilitation: Ava was addicted to prescription painkillers after suffering an ankle injury. She struggled through intense withdrawal symptoms before being admitted into a rehab facility where she found help via holistic approaches like acupuncture, deep breathing exercises and journaling. These treatments allowed Ava, a self-proclaimed skeptic of alternative medicine, to heal along with the standard addiction therapies.
Some Facts About How to Address Co-occurring Disorders in Addiction Treatment:
- Co-occurring disorders, or the presence of both a mental health disorder and substance use disorder, affect a significant portion of individuals seeking addiction treatment. (Source: National Institute on Drug Abuse)
- Integrated treatment, which addresses both the mental health and substance use disorders concurrently, has been demonstrated to improve outcomes for individuals with co-occurring disorders. (Source: Substance Abuse and Mental Health Services Administration)
- Assessment and diagnosis of co-occurring disorders should be a routine part of addiction treatment intake procedures. (Source: Addiction Science and Clinical Practice)
- Effective treatment for co-occurring disorders may involve a combination of medication, therapy, and support groups. (Source: American Psychiatric Association)
- Long-term management and support are crucial for individuals with co-occurring disorders to prevent relapse and maintain recovery. (Source: Substance Abuse and Mental Health Services Administration)
FAQs about How To Address Co-Occurring Disorders In Addiction Treatment
What are co-occurring disorders in addiction treatment?
Co-occurring disorders in addiction treatment are when an individual has both an addiction disorder and a mental health disorder.
How are co-occurring disorders treated in addiction treatment?
Co-occurring disorders are treated in addiction treatment through a combination of therapies that address both the addiction and the mental health disorder simultaneously.
What is the importance of addressing co-occurring disorders in addiction treatment?
Addressing co-occurring disorders in addiction treatment is important because it can lead to relapse or an exacerbation of the mental health disorder.
What kind of therapies are used to address co-occurring disorders in addiction treatment?
The kinds of therapies used to address co-occurring disorders in addiction treatment include cognitive-behavioral therapy, dialectical behavior therapy, and medication-assisted therapy.
Who is qualified to provide addiction treatment for co-occurring disorders?
Those qualified to provide addiction treatment for co-occurring disorders include licensed therapists and psychiatrists who specialize in addiction and mental health treatment..
Is it possible to fully recover from co-occurring disorders in addiction treatment?
Yes, it is possible to fully recover from co-occurring disorders in addiction treatment with proper treatment and ongoing support.